Hum. Reprod.-2006-García-Pérez-880-7
-
Upload
anis-murniati -
Category
Documents
-
view
213 -
download
0
Transcript of Hum. Reprod.-2006-García-Pérez-880-7
-
7/27/2019 Hum. Reprod.-2006-Garca-Prez-880-7
1/8
Human Reproduction Vol.21, No.4 pp. 880887, 2006 doi:10.1093/humrep/dei413
Advance Access publication February 3, 2006.
880 The Author 2006. Published by Oxford University Press on behalf of the European Society of Human Reproduction and Embryology. All rights reserved.For Permissions, please email: [email protected]
Alterations in the phenotype and function of immune cells inovariectomy-induced osteopenic mice
M.A.Garca-Prez
1,7
, I.Noguera
2
, C.Hermenegildo
1,3
, A.Martnez-Romero
4
, J.J.Tarn
5
and A.Cano6
1Research Unit, Hospital Clnico Universitario of Valencia, Av. Blasco Ibez 17, 46010 Valencia, Spain, 2Research Unit, Faculty of
Medicine, University of Valencia, 46010 Valencia, Spain, 3Department of Physiology, Faculty of Medicine, University of Valencia,
46010 Valencia, Spain, 4Department of Biochemistry and Molecular Biology, Faculty of Medicine, University of Valencia, 46010
Valencia, Spain, 5Department of Functional Biology and Physical Anthropology, Faculty of Biological Sciences, University of Valencia,
46100 Burjassot, Spain and 6Department of Pediatrics, Obstetrics and Gynecology, Faculty of Medicine, University of Valencia, 46010
Valencia, Spain
7To whom correspondence should be addressed. E-mail: [email protected]
BACKGROUND: Within the last few years, much evidence has been presented on the involvement of the immune
system in certain types of bone loss, such as activated T cells in rheumatoid arthritis and in periodontitis. Estrogen
deficiency induces bone loss; however, how this deficiency affects the immune system has not been sufficiently stud-
ied. METHODS: To evaluate the effects of estrogen withdrawal on the status and functionality of the immune system,
mice were ovariectomized or sham-operated, and 5 weeks after surgery, when osteopenia had developed, several
parameters were analysed in spleen and in bone marrow. We analysed bone turnover, cell phenotype by flow cytom-
etry, cell function by cell proliferation assays, and the expression of several genes related to the process. RESULTS:
Five weeks after ovariectomy, augmented osteoclastogenesis persisted in the bone marrow. In addition, the ovariect-
omized mice had more B-cells and CD3+ T-cells expressing the receptor activator of NF-kB ligand (CD3+/RANKL+).
The ovariectomized mice had lower serum alkaline phosphatase activity, a normal amount of T cells, lower percentages
of CD11b+ and CD51+ cells in the bone marrow, and a lower serum interferon- level compared with sham-operated
controls. CONCLUSIONS: The data suggest that, 5 weeks after ovariectomy, bone turnover remains imbalanced,
with increased osteoclastogenesis and a decreased rate of bone formation. Moreover, there is an increase in B-cell
formation, with normal and decreased percentages of T cells and myelomonocytic cells (CD11b+), respectively, in the
bone marrow. Decreased serum interferon- levels could be involved in the increased osteoclastogenesis found in thepresent work.
Key words: bone metabolism/estrogen deficiency/immune system/mouse/ovariectomy
Introduction
Recent research has uncovered molecules crucial to bone
metabolism, and in particular to the generation, development
and activation of osteoclasts, the cells that resorb bone. These
molecules include the receptor activator of the NF-B ligand(RANKL, also known as TRANCE, ODF and OPGL), its
receptor RANK, and osteoprotegerin, all of which are keymolecules for osteoclastogenesis. This was demonstrated
through the use of mice deficient in these molecules (Theill
et al., 2002). RANKL and RANK were first described in
immune system cells, where they are expressed in activated T
cells, and in dendritic cells, respectively, and are implicated in
cell survival and immunomodulation (Anderson et al., 1997).
In bone, the binding of RANKL on stromal or osteoblastic
cells to RANK on pre-osteoclasts, together with macrophage
colony stimulating factor (M-CSF), is necessary and sufficient
for the generation, differentiation and activation of osteoclasts
(Lacey et al., 1998), although other molecules in the bone mar-
row environment, such as interleukin (IL)-1, IL-6 and tumour
necrosis factor (TNF)-, intervene in the process (Jilka, 1998).These discoveries have led to the creation of a new field of
research, osteoimmunology (Arron and Choi, 2000).
Much evidence has linked the immune system to bone loss(Theill et al., 2002). Some of this evidence comes from the study
of animal models of rheumatoid arthritis and periodontitis. It has
been demonstrated that activated T cells express RANKL,
which, in turn, is able to stimulate osteoclastogenesis and bone
loss (Kong et al., 1999; Teng et al., 2000). Moreover, estrogen
regulates T-cell functions through an estrogen receptor-mediated
pathway, and T-cell subset alterations were found in postmeno-
pausal women with osteoporosis (Olsen and Kovacs, 1996). Fur-
thermore, it has been shown that ovariectomy induces B-cell
-
7/27/2019 Hum. Reprod.-2006-Garca-Prez-880-7
2/8
Immune system status in osteopenic m
8
lymphopoiesis, and that these cells can be a source of osteoclasts
(Masuzawa et al., 1994; Sato et al., 2001). Therefore, immune
system cells may induce bone loss not only during inflammation
but also under conditions of estrogen deficiency.
Estrogen deficiency induces bone loss and osteoporosis
(Jilka, 1998; Riggs et al., 1998), and since both bone and
immune cells have active receptors for estrogens (Bellido
et al., 1993; Komi and Lassila, 2000; Igarashi et al., 2001) it is
conceivable that estrogen deficiency induces changes not only
in bone but also in the immune system, and that these changes
could be associated with increased osteoclastogenesis and bone
loss. The status of the immune system after estrogen deficiency
is established; however, it needs further study.
In this work, ovariectomy was carried out in the mouse as a
model of estrogen deficiency. Ovariectomy induces a rapid aug-
mentation in bone turnover, causing an increase in both bone
resorption and bone formation (Jilka et al., 1998; Tanizawa et
al., 2000). In the mouse, indices of bone remodelling peak at the
first or second week after ovariectomy and then fall progres-
sively. Five weeks after ovariectomy, bone turnover has been
normalized almost completely, and the mouse has developed
osteopenia due to the large amount of trabecular bone lost (Jilkaet al., 1998; Tanizawa et al., 2000; Miyazaki et al., 2004).
The purpose of the present study was to analyse several
aspects of the immune system in the spleen and bone marrow
in mice that had developed osteopenia as a consequence of
estrogen deficiency induced by ovariectomy. We studied the
phenotype and function of both cellular types, several parame-
ters in serum, such as calcium, alkaline phosphatase (ALP)
activity, TNF-, IL-6 and interferon- levels, and the expres-sion of several genes 5 weeks after ovariectomy, when bone
turnover normalized after an initial imbalance provoked by the
abrupt interruption in the supply of estrogens.
Materials and methods
Media and reagents
Recombinant mouse soluble receptor activator of NF-B ligand
(sRANKL) and recombinant murine M-CSF were obtained from
PeproTech (London, UK). Monoclonal CD3 (clone 1452C11), CD28
(clone 37.51), CD3-fluorescein isothiocyanate (FITC) (clone 145
2C11), CD11b-FITC (clone M1/70), CD4-phycoerythrin (PE) (clone
GK1.5), CD8-PE (clone 536.7), CD51-PE (clone RMV-7), RANKL-
PE (clone IK22/5) and rat PE-negative control (clone KLH/G2a-1-1)
were from e-Bioscience (San Diego, CA). Monoclonal CD19-FITC
(clone 6D5), CD25-RPE (clone PC61.5.3), rat anti-mouse RANK
(clone LOB14-8), rat FITC-negative control (clone LO-DNP-16) and
F(ab)2 goat anti-rat immunoglobulin G-FITC were from Serotec(Oxford, UK).
Cells were obtained in calcium- and magnesium-free phosphate-
buffered saline (PBS; Invitrogen, Carlsbad, CA, USA), and incubated
in phenol red-free RPMI-1640 (spleen cells) or in phenol red-free
Minimum Essential Medium Modified (-MEM) (bone marrow
cells). Media was supplemented with 10% charcoal-stripped, heat-
inactivated fetal bovine serum (FBS), 2 mmol/l glutamine, 100 IU/ml
penicillin G and 100 g/ml streptomycin (all from Gibco, Invitrogen).
Calcitriol (1,25-dihydroxy vitamin D3) was from Alexis (San Diego,CA, USA). PCR primers and enzymes for reverse transcription were
from Invitrogen. All other chemical reagents were from Sigma
(Sigma-Aldrich, St Louis, MO, USA).
Mice
The ethics committee of our institution approved all animal proc
dures. Ten-week-old female C57BL/6 mice (Harlan Interfau
Ibrica, Barcelona, Spain) were subjected to either dorsal ovarie
tomy or sham operation under general anaesthesia by using 150 mg/
of ketamine (Merial, Lyon, France) and 5 mg/kg acepromazi
(Calmo Neosan, Pfizer, NY, USA). Animals were kept at 21C with
12-light:12-h dark cycle and were allowed free access to a pellete
standard mouse laboratory diet containing 0.88% calcium and 0.59
phosphorus (Panlab, Barcelona, Spain) and tap water. The mice wekilled 5 weeks after surgery under halothane anaesthesia (Fluothan
Zeneca, Macclesfield, UK) by cardiac puncture, and the bloo
spleen and femora were removed aseptically. The uterus of ea
mouse was also removed and weighed to confirm the success of ov
riectomy surgery. Blood was allowed to clot and the serum was sep
rated and frozen at 80C until analysis. The spleen and femora weprocessed immediately. None of the mice exhibited evidence
infectious disease, impaired growth (see Results), immunosuppre
sion or other side-effects.
Cell culture
The spleen cells were isolated by careful disintegration of spleen with
scalpel in PBS or by passing the tissue through a sterile 90-m nyl
mesh in PBS. The bone marrow cells were isolated from the femusing centrifugation (Cenci et al., 2000). Briefly, after removal of bon
adherent soft tissues, femur ends were cut off with scissors and insert
into a 0.6-ml microcentrifuge tube with a hole in the bottom and plac
in a 1.5-ml carrier microcentrifuge tube. Cells were extracted from t
bones by centrifugation at 4C and resuspended immediately in PBS.Spleen cells were carefully layered over Histopaque 1077 (Sigm
and centrifuged for 30 min at 400 g at room temperature. Monon
clear cells were collected, washed twice in PBS, resuspended in RPM
containing FBS and then incubated. The bone marrow suspensi
cells were treated similarly, except that they were allowed to adhe
overnight in six-well plastic plates to deplete mature stromal ce
(Dao et al., 1997; Cenci et al., 2000), with the exception of flo
cytometry analysis and RNA extraction, in which this step of adhesi
was omitted. After incubation, non-adherent cells were harvested
pipetting, and mononuclear cells were obtained as described f
spleen cells. Mononuclear non-adherent bone marrow cells we
resuspended in -MEM containing FBS. Spleen and bone marrocells were counted using a haemocytometer, and aliquots of the
cells were used for RNA isolation.
Serum biochemistry
Serum calcium, measured by reaction with o-cresolphthalein, and AL
were assayed using commercial kits (Sigma). Serum levels of TNF-
IL-6, interferon-and IL-2 were measured by an enzyme-linked immnosorbent assay according to the manufacturers instructions (Diaclon
Besanon, France). Total tartrate-resistant acid phosphatase (TRA
was determined by a rapid microplate colorimetric assay with modifictions (Lau et al., 1987).p-Nitrophenyl phosphate (10 mmol/l) was us
as substrate in a buffer containing 100 mmol/l sodium acetate, pH 5
20 mmol/l sodium tartrate and 0.1% (v/v) Triton X-100. Serum sampl
(10 l) were added to 200 l of substrate and incubated at 37C for min. The reaction was stopped by the addition of 100 l 0.5 moNaOH, and absorbance was read at 405 nm with a microplate read
(Model 550, Biop-Rad, Richmond, CA, USA).
Resorption pit assay
Bone marrow preosteoclasts were characterized by assessing the
ability to form resorption pits on calcium phosphate-coated cultu
-
7/27/2019 Hum. Reprod.-2006-Garca-Prez-880-7
3/8
M.A.Garca-Prez et al.
882
wells. For this, 5 104 non-adherent mononuclear bone marrow cellsin -MEM containing 10% FBS were seeded onto calcium phosphate-coated osteological discs (Millenium Biologix, Kingston, Ontario,
Canada) and incubated for 12 days in a humidified atmosphere of 5%
CO2 in air in the presence of vehicle, M-CSF (20 ng/ml) or M-CSF
(20 ng/ml) plus murine sRANKL (20 ng/ml). The medium was
changed three times per week, eliminating half of the medium and
replacing it with fresh medium plus stimuli. After 12 days, adherent
cells were removed with bleach solution (6% NaOCl and 5.2% NaCl).
The discs were examined for the presence of resorption lacunae bylight microscopy after von Kossa staining, according to the manufac-
turers instructions.
Cell proliferation and viability analysis
Cell proliferation and viability were evaluated with an XTT (sodium 3-
[1-(phenylaminocarbonyl)-3,4-tetrazolium]-bis (4-methoxy-6-nitro)
benzene sulfonic acid hydrate)-based colorimetric assay (Roche Diag-
nostics, Mannheim, Germany) according to the manufacturers instruc-
tions. Briefly, 1.5 105 spleen or 4 104 non-adherent bone marrowmononuclear cells in 100 l were placed in 96-well microtitre plates(Orange Scientific, Braine-lAlleud, Belgium) supplemented with
glutamine, antibiotics and 10% FBS at 37C in a humidified atmosphereof 5% CO2 in air for 4 days. The stimuli and their combinations used are
indicated in Table II, and were added in triplicate. After incubation, 50 lof XTT substrate was added to each well and incubated in the conditions
described above. Absorbance of each well was determined at 450 nm
using a microplate reader. Proliferation data in Table II represent the
quotient of proliferation for each stimulus (in triplicate) and proliferation
of the same cells in the same culture plate incubated with vehicle.
Flow cytometry and DNA staining
Cells were labelled with antibodies at the manufacturers recom-
mended dilutions and conditions. Mononuclear spleen and bone mar-
row cells (1 106) were incubated for 30 min on ice with the indicatedantibodies and then washed and resuspended in PBS containing 1%
bovine serum albumin and 0.1% sodium azide. Non-specific signal
was estimated by incubation with rat FITC- and PE-conjugated IgGisotype controls. For analysis of the cell cycle, cells were labelled with
Coulter DNA-Prep (Beckman Coulter, Fullerton, CA, USA) accord-
ing to the manufacturers instructions. Labelled cells were analysed
with an EPICS-XL flow cytometry system (Beckman Coulter). Data
were expressed as the percentage of positive cells since, although ova-
riectomy induced approximately 20% increment in spleen and bone
marrow total cell content, there were no significant differences
between ovariectomized and sham-operated mice.
RNA isolation and semiquantitative RT-PCR
Total RNA was extracted from mononuclear bone or spleen cells with
Trizol reagent (Invitrogen) according to the manufacturers protocol,
and the integrity of the RNA preparations was examined by agarose gel
electrophoresis. One microgram of total RNA was reverse-transcribedin a 20-l reaction volume into single-stranded cDNA with a first-strand cDNA synthesis kit using an oligo-dT primer (Invitrogen). The
subsequent PCR was performed with specific primers for each gene
with Taq polymerase from Sigma. To ensure equal starting quantities
of cDNA for the experiment and to allow the semiquantification of the
PCR products, reverse-transcribed RNA samples were amplified with
primers specific for glyceraldehyde phosphate dehydrogenase (GAPDH).
Amplifications were done using a GeneAmp 9600 thermal cycler (Per-
kin-Elmer), with the temperature cycling set according to the primer
length and Tm value. The number of cycles for each primer pair was
determined according to a linear amplification curve established from
primary experiments. For each PCR reaction, several samples under-
went 1215 extra cycles of amplification to guarantee the semiquantifi-
cation of the experiment. Amplified PCR products were separated on
2% agarose gel and stained with ethidium bromide for visualization.
The intensity of ethidium bromide-stained bands was quantified using
the histogram function in Adobe Photoshop (version 7.0) and was nor-
malized with the GAPDH housekeeping gene.
The sequence of primers used were the following: GAPDH, sense
5-ACC ACA GTC CAT GCC ATC AC-3 and antisense 5-TCC
ACC ACC CTG TTG CTG TA-3; CD25, sense 5-CTC TCC TACAAG AAC GGC AC-3 and antisense 5-TCA CTA GCC AGA AATCGG TGG-3; core binding factor a1 (Cbfa1), sense 5-CCG CACGAC AAC CGC ACC AT-3 and antisense 5-CGC TCC GGC CCACAA ATC TC-3; RANKL, sense 5-CAT TTG CAC ACC TCACCA TC-3 and antisense 5-AAG GGT TGG ACA CCT GAA TG-3; IL-6, sense 5-ATG AAG TTC CTC TCT GCA AGA GAC T-3 and antisense 5-CAC TAG GTT TGC CGA GTA GAT CTC-3;TRAP, sense 5-ACT TCC CCA GCC CTT ACT ACC-3 and anti-sense 5-TCA GCA CAT AGC CCA CAC CG-3; TNF-, sense 5-TCT TCT GTC TAC TGA ACT TCG G-3 and antisense 5-GTAGAG AAT GGA TGA ACA CCC-3; interferon-, sense 5-TCTTGG CTT TGC AGC TCT TCC-3 and antisense 5-CGA ATC AGC
AGC GAC TCC TTT TC-3.
Statistical analysis
Analysis of variance test was used for statistical comparisons between
means of different groups. Results are presented as mean SD. Thenumbers of mice used in each experiment appear in the tables or in the
text of the figures; they correspond to three surgical interventions in
different weeks. A P value < 0.05 of was considered statistically
significant. The entire statistical analysis was carried out using the
Statistical Package for Social Sciences (SPSS, Chicago, IL, USA), v.
11.0 for Windows.
Results
Serum parameters in ovariectomized mice
The success of ovariectomy was determined from the uterine
hypoplasia caused by estrogen deficiency (Table I and Figure 3A).
Ovariectomy induced a dramatic decrease in uterine weight but
not body weight. Ovariectomy increased bone resorption, as
shown by increased values of serum calcium (P < 0.01; Table I).
Serum levels of ALP, a formation marker of bone remodelling,
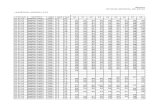
Table I. Physical parameters, biochemical serum values and number ofresorption pits of sham-operated and ovariectomized mice
Data are mean SD corresponding to 1628 mice from two experiments,except for cytokines (1012 mice) and for resorption pit assay (four mice).ALP, alkaline phosphatase; TRAP, tartrate-resistant alkaline phosphatase.
Sham-operated Ovariectomized P
Body weight (g) 22.73 1.41 23.94 2.68 NSUterus weight (mg) 102.06 23.71 21.66 6.41
-
7/27/2019 Hum. Reprod.-2006-Garca-Prez-880-7
4/8
Immune system status in osteopenic m
8
were lower in ovariectomized mice (P < 0.01). Furthermore,
ovariectomy caused a significant decrease in serum levels ofinterferon-(P < 0.01), a T-cell produced cytokine that inhibitsosteoclastogenesis in vitro. Other markers (TNF-, IL-6, IL-2and TRAP) remained unchanged. The number of resorption
pits generated by mononuclear non-adherent ovariectomy bone
marrow cells after incubation with RANKL and M-CSF
was more than twice that found in sham-operated operated
mice (P < 0.05; Table I and Figure 1). The number of pits
formed when cells were incubated with vehicle or M-CSF
alone was very small (
-
7/27/2019 Hum. Reprod.-2006-Garca-Prez-880-7
5/8
M.A.Garca-Prez et al.
884
This agrees with previous work in which an increased number
of osteoclastic cells 5 weeks after ovariectomy was described,
although osteoclastic cell numbers declined over time (Jilka
et al., 1998). Results of the present work show no increases in
serum levels of IL-6 and TFN-, although a trend can beobserved (Table I). Nevertheless, inflammatory cytokines are
involved in the process since it has been reported that blocking
IL-1 and TNF- by antibodies prevents bone loss after ovariec-tomy (Kimble et al., 1995).
Two unexpected results can be seen in Table I: the small
amount of serum ALP-activity and the low level of interferon-after ovariectomy. ALP activity is considered a marker of bone
remodelling (Weaver et al., 1997; Minisola et al., 1998), and a
high correlation exists between bone-specific and total ALP(Takahashi et al., 1997). After ovariectomy, levels of total and
bone-specific ALP increase, peak between the first and second
weeks, and then decline progressively (Tanizawa et al., 2000;
Miyazaki et al., 2004). Although total ALP activity is not
bone-specific, it can be assumed that, if there is no hepatic dis-
ease (Minisola et al., 1998), it should reflect changes caused by
bone marrow cells (Weaver et al., 1997). This decreased level
of ALP activity 5 weeks after ovariectomy implies that bone
formation is impaired, and together with the increase in resorp-
tion pit-generating cells in bone marrow, could explain the
increased calcaemia detected, thus linking estrogen deficiency
with osteoblastic function. We cannot discard the possibility
that the decreased levels of ALP after ovariectomy, however,are related to the low bone density reached by our strain of
mouse (C57BL/6) compared with others, as a consequence of a
lower rate of bone formation (Richman et al., 2001). In accord-
ance with our data, after ovariectomy, decreases have been
described in the percentage of preosteoblastic marrow stromal
cells in early postmenopausal women (Eghbali-Fatourechi
et al., 2003), in serum ALP activity (Sakakura et al., 2001), in
the number of ALP-positive colony-forming units (Pei et al.,
2003) and in ALP activity in individual osteoblasts (Gevers
et al., 2002).
Table II. Cell proliferation analysis of mononuclear spleen and bone marrow cells
PHA, phytohaemagglutinin; Con A, concanavalin A; PMA, 4-phorbol-12-myristate-13-acetate; M-CSF, macrophage colony-stimulating factor; RANKL, receptoractivator of NF-B ligand.Data are mean SD of triplicate determinations corresponding to six mice.aP < 0.05.
Spleen Bone marrow
Sham-operated Ovariectomized Sham-operated Ovariectomized
PHA (10 g/ml) 144.5 18.5 167.1 44.3 131.3 16.5 115.1 9.8Con A (10 g/ml) 222.8 70.5 240.8 41.6 152.5 17.8 128.4 18.9PMA (10 ng/ml) 152.0 32.6 195.6 6.8a 139.3 10.5 127.5 6.6CD3 (2 g/ml) 150.7 61.5 115.4 29.3 106.1 12.2 109.9 12.7CD3 (2 g/ml) + CD28 (0.2 g/ml) 173.5 77.4 156.4 58.4 114.7 3.6 109.7 2.1a
M-CSF (25 ng/ml) 281.2 151.1 406.1 66.0 484.5 149.7 398.4 102.3Calcitriol (0.01 mol/l) 92.7 5.1 100.0 13.5 95.5 7.1 96.8 6.7RANKL (25 ng/ml) 100.9 7.4 104.0 5.7 108.1 16.6 103.5 6.6
Figure 2. Representative flow cytometry dot plots sorted from mice.Forward and side light-scatter plot of unstained cells after Histopaquecentrifugation from spleen (A) and bone marrow (B) cells. The gatedregion contains the greatest number of lymphocytes/blast cells inspleen and bone marrow.
Table III. Flow cytometry analysis of mononuclear spleen cells
Data indicate the percentage of positive cells and are mean SD, correspondingto 412 mice from two different experiments.aP < 0.05.
Molecule Sham-operated Ovariectomized
CD3 32.6 7.8 28.5 8.4CD3+/CD4+ 19.3 2.8 17.4 4.4CD3+/CD8+ 13.5 5.0 11.4 4.4CD11b 12.8 4.2 12.1 2.2CD19 38.7 9.8 46.1 8.6CD25 43.0 9.6 56.7 8.5a
CD51 32.0 5.7 28.5 6.2
Table IV. Flow cytometry analysis of mononuclear bone marrow cells
Data indicate the percentage of positive cells and are mean SD, correspond-ing to 612 mice from two different experiments.aP < 0.05; bP < 0.01.
Molecule Sham-operated Ovariectomized
CD3 8.2 5.2 6.5 2.3
CD19 34.6 6.9 41.0 6.5a
CD11b 30.9 13.8 20.6 8.1a
CD25 23.2 5.9 23.1 3.6CD51 41.5 6.5 35.0 2.3b
RANK 2.8 0.5 3.0 0.6CD3+/RANKL+ 2.1 0.7 4.25 1.4b
-
7/27/2019 Hum. Reprod.-2006-Garca-Prez-880-7
6/8
Immune system status in osteopenic m
8
Interferon- is an in vitro negative regulator of osteoclas-togenesis (Gowen and Mundy, 1986; Takayanagi et al., 2000).
Nonetheless, in vivo interferon-cures osteopetrosis by stimu-lating osteoclast formation and bone resorption (Key et al.,
1995), and interferon- receptor-deficient mice have beenshown to be protected against ovariectomy-induced bone loss
(Cenci et al., 2003). The issue of interferon- is complexbecause this cytokine is likely to have tissue specific effects.
Data in the literature about interferon-production after gona-dectomy are sparse, however, particularly in the bone marrow
microenvironment. Cenci and colleagues have described an
increase in the percentage of CD4+ T cells expressing inter-
feron- and in the interferon- concentration in culture super-
natants of bone marrow CD90+ T cells after ovariectom
concluding that this increase is critical in explaining the bo
effects in estrogen deficiency (Cenci et al., 2003). Howeve
most data indicate that estrogens up-regulate and gonadectom
down-regulates interferon-production, although these studiwere not carried out in bone marrow cells. For instance, it h
been reported that interferon- production is decreased aftmice gonadectomy (Aloisi et al., 2001; Sun et al., 2003), b
up-regulated by estrogen in spleen and lymph node lym
phocytes (Karpuzoglu-Sahin et al., 2001; Maret et al., 2003
Moreover, a decrease in the interferon- production has albeen described in postmenopausal women (Yang et al., 200
Kumru et al., 2004). These data suggest a difference in the re
ulation of interferon- production for T cells from periphertissues (spleen and lymph node) and bone marrow T cells aft
gonadectomy. Although the rationale for such impairme
remains unclear, it might be due to differences between sy
temic and local interferon- production. Indeed, interferonimplicated in osteoclastogenesis should be produced mainly
the bone marrow, and it remains to be demonstrated wheth
the decrease in interferon- production detected in this an
other studies has an effect on the increased osteoclastogenesthat is established after gonadectomy (Teitelbaum, 2004).
Estrogen deficiency induced important changes in cellul
subtypes of spleen and bone marrow. Ovariectomy induced
increase in levels of B-cells (CD19+) in bone marrow an
CD25+ cells (IL-2 receptor chain) in spleen as well as bone marrow (total cells; results not shown). Both estroge
deficiency (this work and Masuzawa et al., 1994) and IL
administration (Miyaura et al., 1997) induce B-lymphopoies
a process that may be involved in the mechanism of stimulat
bone loss. In this respect, it has been reported that B-cells are
source of osteoclasts (Sato et al., 2001). Moreover, an increa
in CD25+ T cells in bone marrow of ovariectomized mi
(Cenci et al., 2003) and of CD25+
and HLA-DR+
T cells postmenopausal women (Yang et al., 2000) has be
described, although this effect has not been well explaine
particularly if IL-2 levels do not change with ovariectom
(Table I).
Estrogen receptors are detectable in the reticular strom
cells of the thymus (Barr et al., 1982), suggesting that estr
gen can modulate T-cell lymphopoiesis. Nevertheless, it is n
clear whether ovariectomy modulates T-cell levels. In th
present study, ovariectomy did not affect T-cell levels (tot
cells or percentage), using a CD3 monoclonal antibody. Th
result agrees with other work, in which it has been reporte
that T cells (Thy 1.2+) do not change (total cells or percentag
after mouse ovariectomy (Masuzawa et al., 1994). Aincrease in bone marrow T-cell content has been describe
after ovariectomy (Cenci et al., 2000; Roggia et al., 2001), b
it is possible that the authors gated immature B cells as T cel
since the CD90 monoclonal antibody used is specific f
CD90.1 (Thy 1.1+) and CD90.2 (Thy 1.2+), and an increase
Thy 1.1+ cells of B-cell lineage after ovariectomy has be
described (Erben et al., 1998b). Results of the present stud
support previous data from other authors showing that ovarie
tomy either does not affect or diminishes mouse and rat bon
marrow T-cell levels (Masuzawa et al., 1994; Erben et a
Figure 3. Uterine hypoplasia and mRNA expression levels in severalgenes assessed by semiquantitative RT-PCR. (A) Marked uterine
hypoplasia is obvious in ovariectomized (right uterus) but not insham-operated mice (left uterus) 5 weeks after surgery. RT-PCR ofRNA samples extracted 5 weeks after surgery from spleen and femursfrom ovariectomized and sham-operated mice. Semiquantitative RT-PCR was performed using the indicated primers in spleen (B) andbone marrow (C) mononuclear cells. The intensity of agarose gelbands are represented, after semiquantitative PCR, calculated asdescribed in Materials and methods. Data are mean SD of duplicatedeterminations corresponding to 12 mice. Photographs representbands of the different PCRs and band length is given as the number ofbase pairs (bp).
-
7/27/2019 Hum. Reprod.-2006-Garca-Prez-880-7
7/8
M.A.Garca-Prez et al.
886
1998a; Safadi et al., 2000), as well as the results of a study in
postmenopausal women (Yang et al., 2000). However, T-cell-
deficient mice do not lose bone after ovariectomy, thus indicating
a determinant role of T-cells in bone loss in estrogen deficiency
(Cenci et al., 2000). Although it is not possible to discard pos-
sible roles of monocytes and NK cells, T cells are responsible
for increased production of pro-resorptive cytokines after ova-
riectomy (Jilka, 1998; Theill et al., 2002), and the decreased
interferon-level found in the present study after ovariectomy.Ovariectomy did not change the percentage of RANK-
expressing cells. RANKL expression in peripheral tissues is
very low (Anderson et al., 1997; Josien et al., 1999). We have
found, however, that levels of bone marrow CD3+/RANKL+
cells are higher after ovariectomy. The increase in RANKL+
T cells could participate in the increased osteoclastogenesis
after ovariectomy, as has been described (Kong et al., 1999).
Percentages of CD11b+ and of CD51+ cells were smaller in
the bone marrow of ovariectomized mice, although, confirm-
ing previous results (Masuzawa et al., 1994), the total cell con-
tent remained unchanged (results not shown). CD11b (Mac-1)
is a marker of the myeloid lineage, while CD51 is directed
against the V-chain of the vitronectin receptor (CD51/CD61,V3) and is considered an osteoclast marker, although it isexpressed in platelets, T cells and granulocytes. Since osteo-
clasts derive from myelomonocytic lineage cells, one could
expect that ovariectomy would increase the monocyte
macrophage precursors in bone marrow. Confirming our
results, a time-course study showed that percentages of
CD11b+ cells and Gr-1+ cells (myeloid cells and granulocytes,
respectively) decreased but B220+ cells (B cells) were
selectively increased 24 weeks after ovariectomy (Masuzawa
et al., 1994). It is possible, though, that the transitory increase
in myeloid precursors is lost or that the osteoclast precursor
represents only a small fraction of CD11b+ and CD51+ cells. In
addition, it is possible that we need a better specific marker todetect increases in osteoclast lineage cells. In this respect, a
transitory increase in ED1+ cells (myeloid marker of monocyte
and osteoclast lineage) has been described 2 weeks after ova-
riectomy coinciding with the up-regulation of osteoclast num-
bers (Erben et al., 1998b; Jilka et al., 1998), the expression
returning to normal after 4 weeks (Erben et al., 1998b).
In the present study, cell functionality was similar in ova-
riectomized and sham-operated mice. Spleen cells from ova-
riectomized mice showed increased proliferation in response to
PMA, a specific activator of protein kinase C (PKC), suggest-
ing that there is an increase in the amount and/or activity of
PKC. In fact, it has been described that the PKC- gene is
upregulated during osteoclastogenesis (Lee et al., 2003).Mononuclear bone marrow cells from ovariectomized mice
exhibited lessened proliferation in response to specific stimula-
tion of T-cells (CD3 + CD28 monoclonal antibodies), which
could be due to impairment of T-cell functionality and could
explain the low level of interferon-observed in this work.Gene expression analysis by RT-PCR did not offer substan-
tial data. The only significant difference found was higher
CD25 expression in bone marrow. Other authors have found
changes in rat osteoprotegerin and RANKL gene expression in
the first days after ovariectomy, but not in the fourth week
(Bonnelye et al., 2002), suggesting that many of the changes in
gene expression occur in the first days after ovariectomy
(Tanizawa et al., 2000; Miyazaki et al., 2004).
In summary, the main effects of estrogen deficiency on the
immune system seem to involve haematopoiesis. It seems that
estrogen receptors are present only in certain immature
immune cells or in a small population of CD8+ T cells and
macrophages (Igarashi et al., 2001). Therefore, the effects of
estrogen could be due to direct action on mature lymphoid cells
or, more probably, through interaction with other estrogen
receptor-expressing cells that can regulate lymphoid cells, such
as dendritic or bone marrow stromal cells (Bellido et al., 1993;
Komi and Lassila, 2000). In bone marrow, ovariectomy up-
regulated CD3+/RANKL+ cells and B cells, did not affect T-cell
levels, and decreased the percentage of myeloid cells, although
only B cells increased in absolute numbers after ovariectomy.
The decrease in serum interferon- level, which can be in thebase of the incremented osteoclastogenesis found, could reflect
impaired T-cell functionality. Furthermore, ovariectomy signi-
ficantly diminished serum ALP activity, indicating a lower rate
of bone formation 5 weeks after ovariectomy.
Acknowledgements
The authors are indebted to Drs Enrique OConnor and GuadalupeHerrera for their expert assistance with flow cytometry, and toMrs Rosa Aliaga and Mrs Elvira Calap for their excellent technicalassistance. This work was supported by grant 01/3051 from the Fondode Investigaciones Sanitarias (FIS).
References
Aloisi AM, Muscettola M and Lupo C (2001) Effects of gonadectomy and painon interferon-gamma production in splenocytes of male and female rats.Brain Behav Immun 15,266272.
Anderson DM, Maraskovsky E, Billingsley WL, Dougall WC, Tometsko ME,Roux ER, Teepe MC, DuBose RF, Cosman D and Galibert L (1997) A
homologue of the TNF receptor and its ligand enhance T-cell growth anddendritic-cell function. Nature 390,175179.
Arron JR and Choi Y (2000) Bone versus immune system. Nature 408,535536.
Barr IG, Khalid BA, Pearce P, Toh BH, Bartlett PF, Scollay RG andFunder JW (1982) Dihydrotestosterone and estradiol deplete corticosen-sitive thymocytes lacking in receptors for these hormones. J Immunol128,28252828.
Bellido T, Girasole G, Passeri G, Yu XP, Mocharla H, Jilka RL, Notides A andManolagas SC (1993) Demonstration of estrogen and vitamin D receptors inbone marrow-derived stromal cells: up-regulation of the estrogen receptorby 1,25-dihydroxyvitamin-D3. Endocrinology 133,553562.
Bonnelye E, Kung V, Laplace C, Galson DL and Aubin JE (2002) Estrogenreceptor-related receptor alpha impinges on the estrogen axis in bone: poten-tial function in osteoporosis. Endocrinology 143,36583670.
Cenci S, Weitzmann MN, Roggia C, Namba N, Novack D, Woodring J andPacifici R (2000) Estrogen deficiency induces bone loss by enhancing T-cellproduction of TNF-alpha. J Clin Invest 106,12291237.
Cenci S, Toraldo G, Weitzmann MN, Roggia C, Gao Y, Qian WP, Sierra Oand Pacifici R (2003) Estrogen deficiency induces bone loss by increasingT cell proliferation and lifespan through IFN-gamma-induced class IItransactivator. Proc Natl Acad Sci USA 100,1040510410.
Dao MA, Hannum CH, Kohn DB and Nolta JA (1997) FLT3 ligand preservesthe ability of human CD34+ progenitors to sustain long-term hematopoiesisin immune-deficient mice after ex vivo retroviral-mediated transduction.Blood 89,446456.
Eghbali-Fatourechi G, Khosla S, Sanyal A, Boyle WJ, Lacey DL and RiggsBL (2003) Role of RANK ligand in mediating increased bone resorption inearly postmenopausal women. J Clin Invest 111,12211230.
Erben RG, Harti G and Graf H (1998a) Ovariectomy does not alter CD4+/CD8+ ratio in peripheral blood T-lymphocytes in the rat. Horm Metab Res30,5054.
-
7/27/2019 Hum. Reprod.-2006-Garca-Prez-880-7
8/8
Immune system status in osteopenic m
8
Erben RG, Raith S, Eberle J and Stangassinger M (1998b) Ovariectomy aug-ments B lymphopoiesis and generation of monocyte-macrophage precursorsin rat bone marrow. Am J Physiol 274,E476E483.
Gevers EF, Loveridge N and Robinson IC (2002) Bone marrow adipocytes: aneglected target tissue for growth hormone. Endocrinology 143,40654073.
Gowen M and Mundy GR (1986) Actions of recombinant interleukin 1, inter-leukin 2, and interferon-gamma on bone resorption in vitro. J Immunol136,24782482.
Igarashi H, Kouro T, Yokota T, Comp PC and Kincade PW (2001) Age andstage dependency of estrogen receptor expression by lymphocyte precur-sors. Proc Natl Acad Sci USA 98,1513115136.
Jilka RL (1998) Cytokines, bone remodeling, and estrogen deficiency: a 1998update. Bone 23,7581.
Jilka RL, Takahashi K, Munshi M, Williams DC, Roberson PK and ManolagasSC (1998) Loss of estrogen upregulates osteoblastogenesis in the murinebone marrow. Evidence for autonomy from factors released during boneresorption. J Clin Invest 101,19421950.
Josien R, Wong BR, Li HL, Steinman RM and Choi Y (1999) TRANCE, aTNF family member, is differentially expressed on T cell subsets andinduces cytokine production in dendritic cells. J Immunol 162,25622568.
Karpuzoglu-Sahin E, Hissong BD and Ansar AS (2001) Interferon-gamma lev-els are upregulated by 17-beta-estradiol and diethylstilbestrol. J ReprodImmunol 52,113127.
Key LL Jr, Rodriguiz RM, Willi SM, Wright NM, Hatcher HC, Eyre DR, CureJK, Griffin PP and Ries WL (1995) Long-term treatment of osteopetrosiswith recombinant human interferon gamma. N Engl J Med 332,15941599.
Kimble RB, Matayoshi AB, Vannice JL, Kung VT, Williams C and Pacifici R(1995) Simultaneous block of interleukin-1 and tumor necrosis factor isrequired to completely prevent bone loss in the early postovariectomyperiod. Endocrinology 136,30543061.
Komi J and Lassila O (2000) Nonsteroidal anti-estrogens inhibit the functional dif-ferentiation of human monocyte-derived dendritic cells. Blood 95,28752882.
Kong YY, Feige U, Sarosi I et al. (1999) Activated T cells regulate bone lossand joint destruction in adjuvant arthritis through osteoprotegerin ligand.Nature 402,304309.
Kumru S, Godekmerdan A and Yilmaz B (2004) Immune effects of surgicalmenopause and estrogen replacement therapy in peri-menopausal women. JReprod Immunol 63,3138.
Lacey DL, Timms E, Tan HL et al. (1998) Osteoprotegerin ligand is a cytokinethat regulates osteoclast differentiation and activation. Cell 93,165176.
Lau KH, Onishi T, Wergedal JE, Singer FR and Baylink DJ (1987) Characteri-zation and assay of tartrate-resistant acid phosphatase activity in serum:potential use to assess bone resorption. Clin Chem 33,458462.
Lee SW, Kwak HB, Chung WJ, Cheong H, Kim HH and Lee ZH (2003) Par-
ticipation of protein kinase C beta in osteoclast differentiation and function.Bone 32,217227.
Maret A, Coudert JD, Garidou L et al. (2003) Estradiol enhances primaryantigen-specific CD4 T cell responses and Th1 development in vivo. Essen-tial role of estrogen receptor alpha expression in hematopoietic cells. Eur JImmunol 33,512521.
Masuzawa T, Miyaura C, Onoe Y, Kusano K, Ohta H, Nozawa S and Suda T(1994) Estrogen deficiency stimulates B lymphopoiesis in mouse bone mar-row. J Clin Invest 94,10901097.
Minisola S, Pacitti MT, Ombricolo E, Costa G, Scarda A, Palombo E andRosso R (1998) Bone turnover and its relationship with bone mineral den-sity in pre- and postmenopausal women with or without fractures. Maturitas29,265270.
Miyaura C, Onoe Y, Inada M, Maki K, Ikuta K, Ito M and Suda T (1997)Increased B-lymphopoiesis by interleukin 7 induces bone loss in mice withintact ovarian function: similarity to estrogen deficiency. Proc Natl Acad Sci
USA 94,93609365.Miyazaki T, Matsunaga T, Miyazaki S, Hokari S and Komoda T (2004)Changes in receptor activator of nuclear factor-kappaB, and its ligand, oste-
oprotegerin, bone-type alkaline phosphatase, and tartrate-resistant acphosphatase in ovariectomized rats. J Cell Biochem 93,503512.
Olsen NJ and Kovacs WJ (1996) Gonadal steroids and immunity. Endocr R17,369384.
Pei W, Bellows CG, Elsubeihi ES and Heersche JN (2003) Effect of ovarietomy on dexamethasone- and progesterone-dependent osteoprogenitorsvertebral and femoral rat bone cell populations. Bone 33,822830.
Richman C, Kutilek S, Miyakoshi N, Srivastava AK, Beamer WG, DonahLR, Rosen CJ, Wergedal JE, Baylink DJ and Mohan S (2001) Postnatal apubertal skeletal changes contribute predominantly to the differences peak bone density between C3H/HeJ and C57BL/6J mice. J Bone Miner R
16,386397.Riggs BL, Khosla S and Melton LJ III (1998) A unitary model for involutio
osteoporosis: estrogen deficiency causes both type I and type II osteoporoin postmenopausal women and contributes to bone loss in aging men. J BoMiner Res 13,763773.
Roggia C, Gao Y, Cenci S, Weitzmann MN, Toraldo G, Isaia G and Pacifici(2001) Up-regulation of TNF-producing T cells in the bone marrow: a kmechanism by which estrogen deficiency induces bone loss in vivo. PrNatl Acad Sci USA 98,1396013965.
Safadi FF, Dissanayake IR, Goodman GG, Jago RA, Baker AE, Bowman ASass DA, Popoff SN and Epstein S (2000) Influence of estrogen deficienand replacement on T-cell populations in rat lymphoid tissues and orgaEndocrine 12,8188.
Sakakura Y, Shide N, Tsuruga E, Irie K and Yajima T (2001) Effects of runing exercise on the mandible and tibia of ovariectomized rats. J BoMiner Metab 19,159167.
Sato T, Shibata T, Ikeda K and Watanabe K (2001) Generation of bonresorbing osteoclasts from B220+ cells: its role in accelerated osteocltogenesis due to estrogen deficiency. J Bone Miner Res 16,22152221.
Sun D, Krishnan A, Zaman K, Lawrence R, Bhattacharya A and Fernandes(2003) Dietary n-3 fatty acids decrease osteoclastogenesis and loss of bomass in ovariectomized mice. J Bone Miner Res 18,12061216.
Takahashi M, Kushida K, Hoshino H, Miura M, Ohishi T and Inoue T (199Comparison of bone and total alkaline phosphatase activity on bone turnver during menopause and in patients with established osteoporosis. CEndocrinol (Oxf) 47,177183.
Takayanagi H, Ogasawara K, Hida S et al. (2000) T-cell-mediated regulatiof osteoclastogenesis by signalling cross-talk between RANKL and IFgamma. Nature 408,600605.
Tanizawa T, Yamaguchi A, Uchiyama Y et al. (2000) Reduction in boformation and elevated bone resorption in ovariectomized rats with specreference to acute inflammation. Bone 26,4353.
Teitelbaum SL (2004) Postmenopausal osteoporosis, T cells, and immune dy
function. Proc Natl Acad Sci USA 101,1671116712.Teng YT, Nguyen H, Gao X, Kong YY, Gorczynski RM, Singh B, Ellen R
and Penninger JM (2000) Functional human T-cell immunity and osteoptegerin ligand control alveolar bone destruction in periodontal infectionClin Invest 106,R59R67.
Theill LE, Boyle WJ and Penninger JM (2002) RANK-L and RANK: T celbone loss, and mammalian evolution. Annu Rev Immunol 20,795823.
Weaver CM, Peacock M, Martin BR, McCabe GP, Zhao J, Smith DL aWastney ME (1997) Quantification of biochemical markers of bone turnver by kinetic measures of bone formation and resorption in young healtfemales. J Bone Miner Res 12,17141720.
Yang JH, Chen CD, Wu MY, Chao KH, Yang YS and Ho HN (2000) Homone replacement therapy reverses the decrease in natural killer cytotoxity but does not reverse the decreases in the T-cell subpopulation interferon-gamma production in postmenopausal women. Fertil Ste74,261267.
Submitted on August 24, 2005; resubmitted on October 21, 2005; accepted November 3, 2005