Hipo e Hiperglicemia en nutrición parenteral
-
Upload
marco-rivera -
Category
Documents
-
view
233 -
download
0
Transcript of Hipo e Hiperglicemia en nutrición parenteral
-
7/28/2019 Hipo e Hiperglicemia en nutricin parenteral
1/15
81
Journal of Parenteral and
Enteral Nutrition
Volume 36 Number 1
January 2012 81-95
2012 American Society for
Parenteral and Enteral Nutrition
10.1177/0148607111418980
http://jpen.sagepub.com
hosted at
http://online.sagepub.com
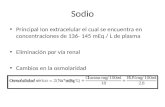
Background
This Clinical Guideline has been developed to guideclinical practice based on the authors assessment of cur-rent published evidence on glycemic control in the neo-nate (within the first month of life) receiving parenteralnutrition (PN). The neonate receiving PN is worthy ofspecial consideration with respect to glucose control, asthis population carries an elevated risk of hyper- andhypoglycemia and may be more susceptible to deleteriouseffects associated with these conditions.
Untreated hyper- or hypoglycemia may lead to unde-sirable clinical outcomes. Prolonged or symptomatichypoglycemia may result in neurodevelopmental impair-ment.1-6 Severe hyperglycemia can lead to osmotic diure-sis resulting in dehydration and electrolyte imbalance.Furthermore there is some evidence to suggest thathyperglycemia in premature infants (particularly thosethat are very low birth weight (VLBW
-
7/28/2019 Hipo e Hiperglicemia en nutricin parenteral
2/15
82 Journal of Parenteral and Enteral Nutrition /Vol. 36, No. 1, January 2012
A.S.P.E.N. Clinical Guidelines has adopted conceptsof the Grading of Recommendations, Assessment,Development and Evaluation (GRADE) working group(http://www.gradeworkinggroup.org). The GRADE work-ing group combined the efforts of evidence analysis meth-odologists and clinical guidelines developers from diversebackgrounds and health organizations to develop anevaluation system that would provide a transparent proc-ess for evaluating the best available evidence and integra-tion of the evidence with clinical knowledge and evenconsideration of patient priorities. These procedures pro-
vide added transparency by developing separate grades for
the body of evidence and for the recommendation. Theprocedures listed below were adopted from the GRADEprocess for use with A.S.P.E.N. Clinical Guidelines withconsideration of the levels of review (by internal andexternal content reviewers, by A.S.P.E.N. and editingexpected for approval by the A.S.P.E.N. Board of Directors.
Three primary stages are involved in developing aClinical Guideline. The first stage is development of spe-cific clinical questions where nutrition support is a rele-
vant mode of therapy, questions to be answered by arigorous review of the published literature. The questionsdeveloped are specific to a life stage group (neonates,pediatrics, adults, geriatrics, pregnancy), in a defineddisease-state or clinical setting, and focused on clinicaloutcomes associated with nutrition support therapy.
The second stage is a transparent process thatdescribes how each research report is evaluated. Finally,a Clinical Guideline recommendation incorporates expertclinical judgment about the context of application of thisresearch into a practice setting with consideration of therelative risks and benefits of doing so.
Pertinent published papers are obtained and appraisedfor evidence quality according to the schema in Tables 1and 2.
The GRADE system combines all the referencesobtained for a given question into a table that is organizedby clinical outcome. The criteria to be used in evaluatingthe quality of the evidence are summarized in Table 2.Consistency, directness, precision and risk of publicationbias are important to include in the assessment of evi-dence quality.17 Inconsistency of randomized controlledtrial (RCT) findings means that the effect size repre-sented by the intervention has a wide confidence interval,
that the effects are conditional (one effect at baselinewith a different effect at a later time point), or that somestudies report a positive and others a negative finding forreasons that cannot be explained by research quality.Indirect evidence might include use of a surrogate out-come (adequate energy intake rather than measuredgrowth in children) or data tangential for the question athand (interpolated from evidence in another age group orcompared to oral diet rather than to parenteral nutrition).Imprecision risk is high when there is no power statementto justify the sample size. The risk of publication bias ishigh when most of the published research reports werefunded by an industry that might benefit from positiveoutcomes reported. Meta-analyses and systematic reviewsmay be used to combine the results of studies to furtherclarify the overall outcome of these studies but will not beconsidered in the grading of the Guideline to avoid con-sidering primary research reports multiple times.
RCT evidence begins with a high rating and observa-tional evidence with a low quality rating. The quality rat-ing may be downgraded due to limitations in study design
Table 1. Evaluation of Study Quality
Randomized Control Trial Quality15
Randomization 1. Was the study described as randomized?2. Was the randomization appropriately performed?
Blinding 3. Was the study double-blinded?4. Were study participants blinded?
5. Was the investigator blinded?Attrition 6. Was the rate of attrition specified and appropriate statistical
treatment (intent-to-treat analysis) employed?Observational Study Quality16
Study Design 7. Were the data collected prospectively?8. How were variables measured?
Power 9. How was sample size determined?Attrition 10. Was the rate of attrition specified and appropriate statistical
treatment employed?Bias 11. How was the study funded?
by guest on March 22, 2013pen.sagepub.comDownloaded from
http://pen.sagepub.com/http://pen.sagepub.com/http://pen.sagepub.com/http://pen.sagepub.com/ -
7/28/2019 Hipo e Hiperglicemia en nutricin parenteral
3/15
A.S.P.E.N. Clinical Guidelines / Arsenault et al 83
or project implementation, to wide confidence intervals,to variable results across studies, indirect evidence orsuspected publication bias. The quality rating may beupgraded if the effect size is very large, a dose-responsegradient is shown, or if all plausible, unreported biases orunmeasured confounders would strengthen the reportedtreatment effect even further (Table 2). When expertopinion is included, the evidence base is assigned a grade
ofvery low and may not be changed.If the evidence grade is high, it is unlikely that furtherresearch will change our confidence in the estimate ofeffect. With moderate grade evidence, further research islikely to modify the confidence in the effect estimate andmay change the estimate. With low grade evidence, furtherresearch is very likely to change the estimate, and with
very low evidence grades, an estimate of the effect is veryuncertain.
A clinical recommendation is then developed by con-sensus of the Clinical Guidelines authors, based on the bestavailable evidence. The risks and benefits to the patient areweighed in light of the available evidence. Conditional lan-guage is used for weak recommendations (Table 3). Thesummary of clinical guidelines for glucose control in neo-nates receiving parenteral nutrition is in Table 4.
Question 1How should blood glucose concentration be determined inneonates? (Tables 5, 6). We suggest that blood glucosescreening be conducted by laboratory serum glucose orglucose electrode measurements rather than point of carereagent test strips when possible (weak).
Rationale. Blood glucose measurements taken with pointof care reagent strips may be susceptible to error due to
Table 2. GRADE Criteria for Grading Evidence for Each Question
Type of Evidence Initial Grade Criteria to Decrease Grade Criteria to Increase GradeFinal Quality
Grade
RCT
OBS
High
Low
Study LimitationsSerious (1) or very serious (2)
limitation to study quality
ConsistencyImportant inconsistency (1)
DirectnessSome (1) or major (2)
uncertainty about directness
PrecisionImprecise or sparse data (1)
Publication biasHigh probability of reporting bias (1)
Strong AssociationStrong evidence of association
significant relative risk of > 2 (< 0.5)
based on consistent evidence fromtwo or more observational studies,with no plausible confounders (+1)
Very strong evidence of associationsignificant relative risk of > 5 (< 0.2)based on direct evidence with nomajor threats to validity (+2)
Dose-response gradientEvidence of a dose response gradient (+1)
Unmeasured ConfoundersAll plausible confounders would have
reduced the effect (+1)
High
Moderate
Low
Very Low
Expert Opinion Very Low Very Low
Adapted from: Grade Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004, 328 (7454): 1490-1494.OBS=observational study; RCT=randomized controlled trial
Table 3. Developing and Grading the Clinical Guideline Recommendation
Quality of Evidence Weighing Risks vs. Benefits GRADE Recommendation Clinical Guideline Statement
High to very low Net benefits outweigh harms Strong We recommendHigh to very low Tradeoffs for patient are important Weak We suggestHigh to very low Uncertain tradeoffs Further research needed We cannot make a
recommendation at this time
Adapted from: Grade Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004, 328 (7454): 1490-1494
by guest on March 22, 2013pen.sagepub.comDownloaded from
http://pen.sagepub.com/http://pen.sagepub.com/http://pen.sagepub.com/http://pen.sagepub.com/ -
7/28/2019 Hipo e Hiperglicemia en nutricin parenteral
4/15
84 Journal of Parenteral and Enteral Nutrition /Vol. 36, No. 1, January 2012
possible contamination of the blood sample with alcoholwhich has been shown to increase the blood glucose read-ing,18 while an elevated hematocrit may falsely lower theresult.19 Additionally glucose measurements obtainedusing reagent test strips measure glucose concentrationsof whole blood and thus have been found to be as muchas 15% lower when compared with laboratory plasmaglucose values.19-20 Plasma glucose measurements have alower standard deviation between repeated values and are
considered the gold standard for monitoring of hypoglyce-mia.19 When it is not possible to utilize plasma glucosemeasurement, the clinician should be aware of thesepotential sources of error associated with point of carereagent test strips.
Question 2
What blood glucose concentration is associated withreduced clinical complications in neonates receiving PN?(Tables 7, 8).We suggest keeping the serum glucose con-centration < 150 mg/dL (weak). We cannot make a rec-ommendation to determine whether serum glucose
should be maintained > 40 mg/dL (recommend furtherresearch). We recommend treating symptomatic hypogly-cemia (strong).
Rationale. Hyperglycemia may occur in the neonatereceiving PN due to excessive glucose infusion rates,stress, or treatment with certain medications includingsteroids and methylxanthines.21 Less effective insulinresponse to elevated blood glucose levels, probable partialinsulin resistance, and a lack of negative feedback on
hepatic glucose production during PN dextrose infusionall make the preterm infant particularly susceptible.21-25
Historically, hyperglycemia has been defined as wholeblood glucose concentration >125 mg/dL or serum glu-cose concentration > 150 mg/dL.21,26 Under this defini-tion, the incidence of hyperglycemia in VLBW infantsduring the first week of life ranges from 40-80%.7,27Multiple studies in neonates (particularly those that arelow birth weight [LBW] and/or premature) have indicated
that persistently elevated serum glucose concentrationsof >150 mg/dL are correlated with adverse clinical out-comes and/or increased mortality.7-9,11,28 Other researchidentifies a link between increased morbidity and mortal-ity and a serum glucose level >180 mg/dL.10 Research inthis area draws correlations between hyperglycemia andmorbidity and mortality, however clinical trials demon-strating causality are lacking.
There is great variability in the definition of neonatalhypoglycemia,29-36 and a lack of research focusing onhypoglycemia in the neonate receiving PN. Hypoglycemiahas been defined as a serum glucose < 40 mg/dL29, but nofirm consensus on this level can be drawn based upon the
current literature. As discussed in a review of currentresearch on subsequent neurodevelopmental outcomesfollowing episodes of hypoglycemia in the first week oflife, there is a need for a well-designed, prospective studyin this area in order to draw accurate conclusions andfirmly establish a clinically-relevant definition for neona-tal hypoglycemia.37
Populations of neonates with increased risk of hypo-glycemia include premature, VLBW, ELBW, small forgestational age (SGA) ( 40 mg/dLRecommend Further Research
We recommend treating symptomatic hypoglycemia. Strong
Question 3: What strategies may be used to maintain optimal blood glucoseconcentration in neonates receiving PN?
We suggest that excess energy and dextrose delivery be avoided. WeakWe suggest that fat emulsion be added to PN infusion. WeakWe recommend against the use of early insulin therapy to prevent
hyperglycemia.Strong
We cannot make a recommendation to evaluate the impact of treating hyper-or hypoglycemia on clinical outcomes.
Recommend Further Research
by guest on March 22, 2013pen.sagepub.comDownloaded from
http://pen.sagepub.com/http://pen.sagepub.com/http://pen.sagepub.com/http://pen.sagepub.com/ -
7/28/2019 Hipo e Hiperglicemia en nutricin parenteral
5/15
85
Table
6.GRADETableQuestion1:H
owshouldbloodglucoseconcentrationbedeterminedinneonates?
Comparison
Outcome
Quantity,TypeEvidence
Findings
EvidenceGRADE
forOutcome
Overall
Recommendation
GRADE
,Rationale
Teststripvs.measuredplasmaglucose
SDorCI
2OBS
Teststripgreater
error
Low
Low
CI=confidenceinterval,OBS=observationalstudy,SD=standarddeviation
Table
5.EvidenceTableQuestion1:Howshouldbloodglucoseconcentra
tionbedeterminedinneonates?
Author,Year(ref#)
StudyDesign,
Qualit
y
Population,
Setting,N
StudyObjective
Results
Comments
Hussain,200019
OBS
Infantsadmittedto
NICUover1y
(N=180)
Comparecapillaryandvenous
glucoseb
yteststripto
laboratory-measuredplasma
glucosevalues
MeandifferenceBetweencapillarytest
stripsandpla
smaglucose,-0.058mmol/L
(SD=1.39)
Betweenvenousteststripandplasma
glucose,0.138mmol/L(SD=0.96)
Confirmsinaccuracyof
whole
bloodglucosetest
stripscomparedto
plasmaglucosevalues
Reynolds,199320
OBS
Infantsadmittedto
NICUover80d
(N=82)
Comparere
agentteststripsto
laboratory-measuredvalues
Reagentteststripshave82-83%
sensitivity,69-70%specificityfor
detectionof
hypoglycemia
CI=confidenceinterval,d=days,NICU=neonatalintensivecareu
nit,OBS=observationalstudy,Ref#=
referencenumber,SD=standarddeviation,y=years
by guest on March 22, 2013pen.sagepub.comDownloaded from
http://pen.sagepub.com/http://pen.sagepub.com/http://pen.sagepub.com/http://pen.sagepub.com/ -
7/28/2019 Hipo e Hiperglicemia en nutricin parenteral
6/15
86
Table7.EvidenceTableforQuestion2:Whatbloodglucoseconcentration
isassociatedwithreducedclinical
complic
ationsinneonatesreceivingPN?
Author,Year
(ref#)
StudyDesign,
Quality
Population,
Setting,N
StudyObjective
Results
Comments
HyperglycemiaStudies
Heimann,
200711
OBS
Largesamplesize
Retrospectiverecord
review
PrematureVLBW
infants27.4(24-
35)weeksGA
withpersistently
elevatedplasma
glucose(N=252)
Evaluatem
ortalityrelatedtomoderate
hyperglyc
emiadefinedas1-3glucose
measures
>150mg/dL(n=125),
severehy
perglycemiadefinedas4
glucosem
easures>150mg/dL(n=45)
relativetonormoglycemicwithno
serumglucosemeasure>150mg/dL
(n=82)
Mortality:
Normoglycemia,13.4%
Moderatehyperglycemia,7.2%
Severehyperglycemia,22.2%
Nonsurvivorshadlower(