MIRTA VARGAS DE ARGENTINA MEDIA 9 CALZADA Cat B 2° grupo 1ª Actividad
FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf
-
Upload
lukebaggio -
Category
Documents
-
view
215 -
download
0
Transcript of FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf

8/19/2019 FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf
http://slidepdf.com/reader/full/farmacocineticaydinamicadelosatbpdf 1/12
Clin Pharmacokinet 2005; 44 (3): 305-316ORIGINAL RESEARCH ARTICLE 0312-5963/05/0003-0305/$34.95/0
© 2005 Adis Data Information BV. All rights reserved.
Pharmacokinetic/PharmacodynamicEvaluation of AntimicrobialTreatments of OrofacialOdontogenic Infections
Arantxa Isla,1 Andr´ es Canut,2 Alicia R. Gasc´ on,1 Alicia Labora,2 Bruno Ardanza-Trevijano,3 Maria ´ Angel´ es Solin´ is1 and Jose Luis Pedraz1
1 Laboratory of Pharmacy and Pharmaceutical Technology, Faculty of Pharmacy, University of
the Basque Country, Vitoria-Gasteiz, Spain
2 Microbiology Unit, Santiago Apostol Hospital, Vitoria-Gasteiz, Spain
3 Maxillofacial Unit, Santiago Apostol Hospital, Vitoria-Gasteiz, Spain
Objective: To evaluate the efficacy of antimicrobial therapy in oral odontogenicAbstractinfections using estimated pharmacokinetic/pharmacodynamic parameters or effi-
cacy indices, and to compare pharmacokinetic/pharmacodynamic breakpoints
with National Committee for Clinical Laboratory Standards’ (NCCLS)
breakpoints.
Study design: Retrospective literature search to obtain minimum inhibitory
concentration (MIC) values, pharmacokinetic parameters of antimicrobials and
NCCLS breakpoints. Pharmacokinetic simulations were carried out using Win-
Nonlin software (Pharsight Corporation, Mountain View, CA, USA).
Methods: For antimicrobials with time-dependent activity, the time that the
plasma drug concentration exceeds the MIC as the percentage of dose interval at
steady state was calculated. For antimicrobials with concentration-dependent
activity, the total area under the plasma concentration-time curve over 24 hours at
steady state divided by the MIC was calculated. Pharmacokinetic/pharmacody-
namic breakpoints were calculated according to these parameters.
Results: Only amoxicillin/clavulanic acid and clindamycin showed adequate
efficacy indices against the most commonly isolated bacteria in odontogenic
infections. Metronidazole reached good indices against anaerobes only.
Pharmacokinetic/pharmacodynamic susceptibility breakpoints do not coincide
exactly with NCCLS breakpoints.
Conclusion: Owing to the scarcity of double-blind, clinical trials on the use of
antimicrobials in endodontics, this study may be useful in determining the best
antimicrobial treatment in these infections. However, as we have not used

8/19/2019 FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf
http://slidepdf.com/reader/full/farmacocineticaydinamicadelosatbpdf 2/12
306 Isla et al.
concentration data in infected tissue to determine pharmacokinetic/pharmacody-
namic indices, it would be necessary to design clinical trials in order to confirm
these results.
Systemic antimicrobial treatment can be a power- double-blinded clinical trials on the use of an-
ful tool for the therapeutic management of timicrobials in endodontics that provide conclusive
dentoalveolar infections, gingivitis and periodontal evidence of therapeutic benefit.[1] As a result, anti-
diseases.[1] Many dentists prescribe antimicrobials microbial usage in endodontics is almost totally
to minimise the risk of infection, ensure the efficacy empirical.[2]
of the treatment, shorten infection periods or mini- Empirical therapy should be based on the most
mise associated risks; however, there is clear evi- common microorganisms isolated and on the effica-dence that these drugs have been overused by den- cy of the treatments. There is a lot of information in
tists for a variety of conditions.[2] Recent studies the literature about the bacteria isolated from pa-
have shown that general dental practitioners in dif- tients with orofacial odontogenic infections, but not
ferent countries prescribe antimicrobials inappropri- many clinical analyses comparing the efficacy of
ately, both therapeutically and prophylactically (e.g. different antimicrobial treatments for these infec-
some odontogenic infections can be managed with- tions have been carried out. Owing to the serious-
out the use of antimicrobials – by tooth extraction, ness of the problems associated with the inappropri-
surgical treatment, endodontic therapy, etc.).[3] They ate use of antimicrobials, especially bacterial resis-
have also demonstrated lack of knowledge about the tance, it is very important to know the efficacy of thedevelopment of multi-resistant bacterial strains.[4-11] antimicrobial treatments in order to select the most
adequate agent for each situation.The rational use of antimicrobials must be based
upon three variables: a defined indication, the ap- Interest in the pharmacokinetic/pharmacodynam-
propriateness of the antimicrobial, and the adverse ic relationships used to describe the antimicrobial
effects associated with the drug. The first factor is activity of antimicrobial agents has recently in-
important because the practitioner needs to be aware creased. It is well known that the final response to
that antimicrobials are not an alternative to dental antimicrobial treatment depends not only on the
intervention, but rather an adjunct to it. Each patient susceptibility of the infecting bacteria, but also on
should be assessed and antimicrobials prescribed other factors that should be taken into account, such
only when necessary because indiscriminate pre- as the pharmacokinetic profile of the chosen anti-
scription can cause drug resistance, which is an infective agent.
emerging and significant problem with oral micro- Schentag et al.[12] defined the clinical practice
organisms.[2] that considers the antimicrobial activity and
In order to select the most effective antimicrobial pharmacokinetic profile of the drug to optimise the
therapy for a patient, isolation and identification of dosage as ‘dual individualisation’. This practice
the involved microorganism should be made. How- uses different mixed parameters (named efficacy
ever, the microflora associated with odontogenic indices) to provide information about the potential
infections is complex, and culture and sensitivity efficacy of the treatment. These indices are based on
testing are not routinely recommended for endodon- both microbiological (pharmacodynamic) andtic procedures. Moreover, there are few controlled, pharmacokinetic parameters. The time that the plas-
© 2005 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2005; 44 (3)

8/19/2019 FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf
http://slidepdf.com/reader/full/farmacocineticaydinamicadelosatbpdf 3/12
PK/PD of Antimicrobials in Odontogenic Infections 307
ma drug concentration exceeds the minimum inhibi- Methods
tory concentration (MIC) as a percentage of the dose
interval at steady state (tss(%)>MIC) has been report- Data Acquisitioned as the best predictor of efficacy for antimicrobials
with time-dependent antimicrobial activity. On the The bibliographical search was made using theother hand, for drugs with concentration-dependent WINSPIRS computer system. Information about thebactericidal activity, the total area under the plasma 90% MIC (MIC90) values of the most commonlyconcentration-time curve (AUC) over 24 hours at prescribed antimicrobials for the pathogens moststeady state divided by the MIC (AUC24,ss /MIC) has frequently isolated in odontogenic infections werebeen reported as the best parameter.[13-19]
collected (table I). These antimicrobials were amox-
Dual dosage individualisation has become an im- icillin (alone and with clavulanic acid), azithro-
portant instrument in deciding the treatment to be mycin, cefuroxime axetil, clindamycin, erythromy-used for patients with different disease states.[12] cin, spiramycin, levofloxacin, metronidazole, mino-
Therefore, the aim of this work was the application cycline and phenoxymethylpenicillin (penicillin V).
of pharmacokinetic/pharmacodynamic parameters The strains of viridans group streptococci, Peptos-
in the prediction of the effectiveness of antimicrobi- treptococcus spp., Prevotella intermedia and
al therapy in oral odontogenic infections. We also Fusobacterium nucleatum were divided into two
estimated the pharmacokinetic/pharmacodynamic groups, as done by Kuriyama et al.:[3] benzylpenicil-
susceptibility breakpoints, which allowed us to pre- lin (penicillin G)-susceptible strains and
dict the efficacy of an antimicrobial treatment benzylpenicillin-resistant strains. A different MIC
against a pathogen if its MIC value is known. We value for each group was considered. All
have also compared these breakpoints with the Na- Porphyromonas gingivalis were judged as ben-
tional Committee for Clinical Laboratory Standards’ zylpenicillin susceptible because they do not pro-
(NCCLS) breakpoints that are normally used in duce β-lactamase. The pharmacokinetic parameters
microbiology laboratories. of these antimicrobials in healthy Caucasian volun-
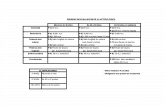
Table I. Ninety percent minimum inhibitory concentration (MIC90) values (mg/L) of antimicrobials for pathogens responsible for odontogenic
infectionsa
Antimicrobial Viridans group Peptostreptococcus Prevotella Porphyromonas Fusobacterium
streptococci[3,20,21] spp.[3,21-24] intermedia [3,21,25-27] gingivalis [3,21,25-27] nucleatum [3,21,25-27]
PS PR PS PR PS PR PS PS PR
Amoxicillin 1 0.25 16 16 8
Amoxicillin/clavulanic acid 1 0.25 2 2 2
Azithromycin 0.12 16 2 1 1 4
Cefuroxime axetil 4 16
Clindamycin 0.5 0.5 2 0.01 0.06 0.03 0.12
Erythromycin 0.06 2 8 64 1 32 0.25 64
Levofloxacin 8 1 8 4 1 4
Metronidazole >128 2 2 2 8
Minocycline 0.5 2 2 4 0.12 8 2 1 2
Phenoxymethylpenicillin 0.25 2 32 0.12 1
(penicillin V)
Spiramycin 0.5 2 0.1 0.2 16
a When more than one MIC90 value was available, the highest one was selected.PR = benzylpenicillin-resistant strains; PS = benzylpenicillin (penicillin G)-susceptible strains.
© 2005 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2005; 44 (3)

8/19/2019 FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf
http://slidepdf.com/reader/full/farmacocineticaydinamicadelosatbpdf 4/12
308 Isla et al.
ised by a time-dependent bactericidal activity, the
tss(%)>MIC was calculated. These data were ob-
tained using the Derive computer system (Derive4.11 for Windows, Soft Warehouse, Inc., HI, USA).
This software allowed us to calculate, from the
corresponding concentration-time equation, a time
interval above a certain drug concentration (MIC)
that is expressed as a percentage of the dose interval.
Treatment with the penicillins was considered effec-
tive when tss(%)>MIC was higher than 40%, and for
the other time-dependent bactericidal drugs, when
this efficacy index was higher than 50%.[60] Al-
though these values had been defined in the litera-
ture for aerobes, in this evaluation they have been
used for both aerobes and anaerobes.
For concentration-dependent bactericidal drugs
such as azithromycin, levofloxacin, metronidazole
and minocycline, the AUC24,ss /MIC was calculated.
For nonsevere infections or infections in immu-
Table II. Pharmacokinetic parameters of the antimicrobials most
commonly prescribed in odontogenic infections[28-59]
Antimicrobial Vd/F ka kel
(L) (h–1) (h–1)β-Lactams
Amoxicillin 29.3 1.68 0.693
Cefuroxime axetil 50.0 1.60 0.495
Phenoxymethylpenicillin 60.0 2.68 0.693
(penicillin V)
Macrolides
Azithromycin 1890.0 0.69 0.034
Erythromycin 100.0 0.70 0.404
Spiramycin 1000.0 0.87 0.088
Lincosamides
Clindamycin 68.9 1.51 0.244
Fluoroquinolones
Levofloxacin 105.95 2.10 0.100
Nitroimidazoles
Metronidazole 49.5 4.07 0.083
Tetracyclines
Minocycline 84.4 2.30 0.040
k a = absorption rate constant; k el = elimination rate constant; Vd/F
= apparent volume of distribution/bioavailability.
nocompetent hosts, in order for treatment to be
successful with these kinds of antimicrobials it is
teers defining a one-compartment model were also necessary to reach an AUC24,ss /MIC ratio highertaken from the literature (table II). Simulations of than 25.[60] In other cases (in more severe infections
the plasma concentration-time curves for the mostor those in immunocompromised hosts) the
common regimens used with each antimicrobial (ta-AUC24,ss /MIC ratio should be higher than 100.[60]
ble III) were carried out with the WinNonlinThese values had been obtained studying aerobic
pharmacokinetic computer system (WinNonlinbacteria, but in this study they have also been used
Standard 1.1, Pharsight Corporation, Mountainfor anaerobes.
View, CA, USA) using the pharmacokinetic param-
eter values given in table II. A one-compartment
Pharmacokinetic/Pharmacodynamicopen model for oral administration with first-order
Breakpoints and National Committee forabsorption and first-order elimination was fitted. At
Clinical Laboratory Standards’ Breakpointsleast eight doses were introduced to simulate steady-
state conditions. AUC was calculated using the trap-
ezoidal rule. If the MIC90 of a strain or group of strains of
bacteria is at or below the breakpoint, or antimicro-
bial concentration, the bacteria will be susceptible toEstimation of Efficacy Indices and
the antimicrobial, and if the MIC90 is above thisEfficacy Criteria
breakpoint the pathogen will be resistant to it.
For amoxicillin (alone and with clavulanic acid), For antimicrobials with time-dependent activity,
cefuroxime axetil, clindamycin, erythromycin, the breakpoint was established by calculating thespiramycin and phenoxymethylpenicillin, character- concentration for which plasma concentrations re-
© 2005 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2005; 44 (3)

8/19/2019 FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf
http://slidepdf.com/reader/full/farmacocineticaydinamicadelosatbpdf 5/12
PK/PD of Antimicrobials in Odontogenic Infections 309
mained above that value during 40–50% of the The NCCLS breakpoints were taken from the
dosage interval. literature.[61,62]
For antimicrobials with concentration-dependentResultsactivity, the breakpoint was calculated using the
following equation 1:Tables IV and V show the values of tss(%)>MIC
PK/PDbreakpoint = AUC24,ss /25calculated for antimicrobials with time-dependent
activity, and AUC24,ss /MIC values for drugs with
concentration-dependent activity, respectively,
against viridans group streptococci, Peptostrepto-
coccus spp., P. intermedia, P. gingivalis and F.
nucleatum.
As can be seen in table IV, the usual regimens of
phenoxymethylpenicillin, amoxicillin, cefuroxime
axetil, erythromycin and spiramycin were not able
to reach plasma concentrations above the MIC val-
ues for all pathogens included in this study for
40–50% of the dosage interval. Amoxicillin only
reached the needed value (40%) against Gram-posi-
tive bacteria (viridans group streptococci and
Peptostreptococcus spp.). Phenoxymethylpenicillin
did not reach a tss(%)>MIC value higher than 40%for P. intermedia. Cefuroxime axetil did not exceed
the MIC during 50% of the dose interval against
Gram-positive bacteria. For Gram-negative patho-
gens, there were no MIC data available in the litera-
ture. Erythromycin and spiramycin did not exceed
the value of 50% against Peptostreptococcus spp. or
F. nucleatum with either of the regimens.
Plasma concentrations of amoxicillin/clavulanic
acid were above the MIC of all bacteria during the
necessary time when administering at least 500mg
three times daily or 1000mg twice daily. In the case
of clindamycin, it was necessary to administer at
least 300mg three times daily in order to reach
adequate concentrations.
None of the regimens of the antimicrobials with
concentration-dependent activity had AUC24,ss /
MIC values that were higher than 25 for all bacteria.
Metronidazole reached good efficacy indices
against all anaerobes (Peptostreptococcus spp., P.intermedia, P. gingivalis and F. nucleatum), but
Table III. Oral dosage regimens considered for the evaluation of
the antimicrobial efficacy against pathogens most commonly isolat-
ed in odontogenic infections
Antimicrobial Dosage
(mg)β-Lactams
Amoxicillin 500 bid/tid
875 bid/tid
1000 bid/tid
Amoxicillin/clavulanic acid 500 bid/tid
875 bid/tid
1000 bid/tid
Cefuroxime axetil 250 bid
500 bid
1000 bid
Phenoxymethylpenicillin (penicillin V) 500 tid/qid
1000 tid/qid
Macrolides
Azithromycin 500 od
Erythromycin 250 bid
500 od/bid/tid
Spiramycin 500 bid/tid
1000 bid
2000 bid
Lincosamides
Clindamycin 150 qid
300 tid/qid600 tid
Fluoroquinolones
Levofloxacin 500 od/bid
Nitroimidazoles
Metronidazole 250 bid/tid
400 bid/tid
500 bid/tid
750 bid/tid
Tetracyclines
Minocycline 100 od/bid
bid = twice daily; od = once daily; qid = four times daily; tid = threetimes daily.
© 2005 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2005; 44 (3)

8/19/2019 FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf
http://slidepdf.com/reader/full/farmacocineticaydinamicadelosatbpdf 6/12
310 Isla et al.
failed for the viridans group streptococci. Azithro- and penicillin-resistant P. intermedia when adminis-
mycin only reached an adequate AUC24,ss /MIC tering minocycline 100mg twice daily.
value against penicillin-susceptible viridans group Table VI shows the calculated pharmacokinetic/ streptococci; levofloxacin only against penicillin-
pharmacodynamic breakpoints of oral pathogens tosusceptible Peptostreptococcus spp. and P.
time-dependent and concentration-dependent bacte-gingivalis. Adequate values were not reached
against penicillin-resistant Peptostreptococcus spp. ricidals. This table also summarises differences be-
Table IV. Time that the plasma drug concentration exceeds the 90% minimum inhibitory concentration as the percentage of dose interval at
steady state (tss(%)>MIC90) for the antimicrobials with time-dependent activity
Antimicrobial Dosage Viridans group Peptostreptococcus Prevotella Porphyromonas Fusobacterium
streptococci spp. intermedia gingivalis nucleatum
(mg) PS PR PS PR PS PR PS PS PR
Phenoxymethylpenicillin 500 qid 91.8 40.1 0.0a 100 57.9
(penicillin V) 1000 qid 100 57.9 0.0a 100 75.0
500 tid 68.6 29.8a 0.0a 81.9 43.1
1000 tid 81.2 43.1 0.0a 94.5 56.0
Amoxicillin 500 tid 60.3 85.8 0.0a 0.0a 12.5a
875 tid 70.7 95.9 0.0a 0.0a 29.5a
1000 tid 73.1 98.3 12.5a 12.5a 32.6a
500 bid 40.1 57.1 0.0a 0.0a 8.2a
875 bid 47.0 63.9 0.0a 0.0a 19.5a
1000 bid 48.7 65.5 8.2a 8.2a 21.6a
Amoxicillin/clavulanic acid 500 tid 60.3 85.8 47.0 47.0 47.0
875 tid 70.7 95.9 58.7 58.7 58.71000 tid 73.1 98.3 60.3 60.3 60.3
500 bid 40.1 57.1 31.3a 31.3a 31.3a
875 bid 47.0 63.9 38.4a 38.4a 38.4a
1000 bid 48.7 65.5 40.1 40.1 40.1
Cefuroxime axetil 250 bid 0.0a 0.0a ND ND ND
500 bid 17.6a 0.0a ND ND ND
1000 bid 32.0a 0.0a ND ND ND
Erythromycin 500 qid 100 55.8 0.0a 0.0a 98.3 0.0a 100 0.0a
500 tid 100 34.3a 0.0a 0.0a 69.3 0.0a 100 0.0a
500 bid 100 19.3a 0.0a 0.0a 44.2a 0.0a 78.0 0.0a
500 od 54.2 9.1a 0.0a 0.0a 21.8a 0.0a 38.8a 0.0a
250 bid 94.0 0.0a 0.0a 0.0a 19.3a 0.0a 62.0 0.0a
Spiramycin 500 tid 100 0.0a 100 100 0.0a
500 bid 44.5a 0.0a 100 100 0.0a
1000 bid 100 0.0a 100 100 0.0a
2000 bid 100 44.5a 100 100 0.0a
Clindamycin 150 qid 100 100 16.9a 100 100 100 100
300 qid 100 100 100 100 100 100 100
300 tid 100 100 100 100 100 100 100
600 tid 100 100 100 100 100 100 100
a tss(%)>MIC value <40% for penicillins and <50% for other antimicrobials.
bid = twice daily; ND = not determined; od = once daily; PR = benzylpenicillin-resistant strains; PS = benzylpenicillin (penicillin G)-
susceptible strains; qid = four times daily; tid = three times daily.
© 2005 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2005; 44 (3)

8/19/2019 FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf
http://slidepdf.com/reader/full/farmacocineticaydinamicadelosatbpdf 7/12
PK/PD of Antimicrobials in Odontogenic Infections 311
Table V. Area under the plasma concentration-time curve over 24 hours at steady state divided by the 90% minimum inhibitory
concentration (AUC24,ss /MIC90) for the antimicrobials with concentration-dependent activity
Antimicrobial Dosage (mg) Viridans group Peptostreptococcus Prevotella Porphyromonas Fusobacterium
streptococci spp. intermedia gingivalis nucleatum PS PR PS PR PS PR PS PS PR
Azithromycin 500 od 64.8 0.5a 3.9a 7.8a 7.8a 2.0a
Levofloxacin 500 bid 11.8a 94.4 11.8a 23.6a 94.4 23.6a
500 od 5.8a 46.7 5.8a 11.7a 46.7 11.7a
Metronidazole 250 tid 1.4a 91.3 91.3 91.3 22.8a
400 tid 2.3a 146 146 146 36.5
500 tid 2.9a 183 183 183 45.6
750 tid 4.3a 274 274 274 65.8
250 bid 1.0a 60.9 60.9 60.9 15.2a
400 bid 1.5a 97.4 97.4 97.4 24.3a
500 bid 1.9a 122 122 122 30.4
750 bid 2.9a 183 183 183 45.6
Minocycline 100 bid 117 29.3 29.3 14.7a 488 7.3a 29.3 58.7 29.3
100 od 58.7 14.7a 14.7a 7.3a 244 3.7a 14.7a 29.3 14.7a
a An AUC24,ss /MIC <25 is required for treatment to be successful in nonsevere infections or infections in immunocompetent hosts.
bid = twice daily; od = once daily; PR = benzylpenicillin-resistant strains; PS = benzylpenicillin (penicillin G)-susceptible strains; tid = three
times daily.
tween NCCLS and pharmacokinetic/pharmacody- upsets. The best dosage option with clindamycin is
namic breakpoints. 300mg three times daily, which is the smallest ade-
quate dosage of this drug. The use of higher dosages
Discussion is not necessary because the risk of adverse effects
would be increased. None of the antimicrobials withAs mentioned in the introductory section, culture
concentration-dependent activity reached adequateand sensitivity testing are not routinely performed
efficacy indices against the five bacteria, althoughfor endodontic procedures; therefore, the spectrum
metronidazole obtained good indices against all an-of the selected antimicrobial should cover the most
aerobes.common microorganisms associated with these
Breakpoints indicate whether or not a microorga-kinds of infections. Amoxicillin/clavulanic acid andnism is susceptible or resistant to an antimicrobialclindamycin are the antimicrobials that provide thetreatment. If the MIC has the same value or isbetter efficacy indices for orofacial infectionssmaller than the pharmacokinetic/pharmacodynam-caused by the most common pathogens isolated inic breakpoint, the microorganism will be suscepti-this localisation, as shown in tables IV and V. Al-
ble, otherwise the treatment will be ineffective. Forthough there are different amoxicillin/clavulanic ac-
example, when amoxicillin 500mg three times dailyid regimens that could be used (500mg three times
is administered, plasma concentrations are above 2daily, 875mg three times daily, 1000mg three times
mg/L during the 40% of the dosage interval (3.2daily and 1000mg twice daily), we consider that
hours), therefore that regimen will be useful against1000mg twice daily would be the best option be-
microorganisms with an MIC value of ≤2 mg/L.cause it is more convenient for the patient owing to
When the concentration-dependent antimicrobialits 12-hour dosage interval (versus an 8-hour dosage
metronidazole is administered at a dosage of 250mginterval), and because it minimises the clavulanicacid dose, thus decreasing the risk of gastrointestinal three times daily, the AUC24,ss is 182.5 mg • h/L. In
© 2005 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2005; 44 (3)

8/19/2019 FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf
http://slidepdf.com/reader/full/farmacocineticaydinamicadelosatbpdf 8/12
312 Isla et al.
Table VI. Comparison of pharmacokinetic/pharmacodynamic (PK/PD) and National Committee for Clinical Laboratory Standards’ (NCCLS)
breakpoints for oral pathogens to time-dependent and concentration-dependent bactericidals
Antimicrobial Dosage (mg) PK/PD breakpoint (mg/L) NCCLS breakpoint (mg/L)a
[all organisms] Streptococcus spp.b (S/R) anaerobesc (S/R)
Amoxicillin 500 tid 2 0.25/8 4/16
875 tid 4
1000 tid 4
500 bid 1
875 bid 1
1000 bid 2
Amoxicillin/clavulanic acid 500 tid 2 2/8
875 tid 4
1000 tid 4
500 bid 1
875 bid 11000 bid 2
Cefuroxime axetil 250 bid 0.25
500 bid 0.5
1000 bid 1
Clindamycin 150 qid 1 0.25/1 2/8
300 qid 2
300 tid 2
600 tid 4
Erythromycin 250 bid 0.25
500 bid 0.5
500 qid 2500 tid 1
500 od 0.06
Spiramycin 500 tid 0.5
500 bid 0.25
1000 bid 0.5
2000 bid 1
Phenoxymethylpenicillin (penicillin V) 500 qid 2 0.12/4 0.5/2
1000 qid 4
500 tid 1
1000 tid 2
Azithromycin 500 od 0.25 0.5/2
Levofloxacin 500 bid 2 2/8
500 od 1
Metronidazole 250 tid 4 8/32
400 tid 8
500 tid 8
750 tid 16
250 bid 4
400 bid 4
500 bid 8
Continued next page
© 2005 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2005; 44 (3)

8/19/2019 FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf
http://slidepdf.com/reader/full/farmacocineticaydinamicadelosatbpdf 9/12
PK/PD of Antimicrobials in Odontogenic Infections 313
Table VI. Contd
Antimicrobial Dosage (mg) PK/PD breakpoint (mg/L) NCCLS breakpoint (mg/L)a
[all organisms] Streptococcus spp.b (S/R) anaerobesc (S/R)
750 bid 8
Minocycline 100 bid 2
100 od 1
a NCCLS breakpoints are applicable for all dosages of the particular drug.
b NCCLS does not have a specific breakpoint for viridans group streptococci.
c NCCLS does not have a specific breakpoint for Peptostreptococcus spp., Prevotella intermedia, Porphyromonas gingivalis and
Fusobacterium nucleatum . These bacteria are anaerobes; therefore, we have considered the breakpoint for anaerobes.
bid = twice daily; od = once daily; qid = four times daily; S/R = sensitive/resistant; tid = three times daily.
order to obtain an AUC24,ss /MIC ratio of 25, the spiramycin[66] and minocycline[67] reach higher con-
MIC value must be 4 mg/L, therefore 4 mg/L will be centrations in gingiva than in plasma. For thesethe pharmacokinetic/pharmacodynamic breakpoint. antimicrobials, if we consider the concentration in
When the MIC value of the pathogen is ≤4 mg/L, the gingival fluid, efficacy indices would be better
this regimen will be adequate. than those calculated by using plasma concentra-
tions. This means that we cannot totally reject theseOur pharmacokinetic/pharmacodynamic break-
antimicrobials when considering the results ob-points do not coincide exactly with NCCLS suscep-
tained in our study. In the case of metronidazole,tibility breakpoints. This may be attributable to dif-
there are some investigators that have found higherferent causes:
concentrations in gingiva than in plasma,[68] but in• NCCLS has not established specific data for eachother studies gingival concentrations were equal tobacterium. Values have been taken from thethose in blood.[69] Macrolides are preferentially tak-breakpoint data given to Streptococcus other thanen up by phagocytes and fibroblasts; therefore, theseS. pneumoniae and also to anaerobes.cells could act as a reservoir and release drugs
• NCCLS values are established without takingslowly in infected tissues,[64,70] resulting in a longerchanges in dosage regimen into account.exposure time to the antimicrobial.
In our study we have used plasma drug concen-
When the pathological process progresses, treat-tration data. We have not taken into account the
ment must be established in a different way. Pulpalantimicrobial concentration in the gingival tissue
infection is an acute process that may cause invasionand this must be considered in order to carry out a
of the periapical area (periapical abscess) or themore appropriate evaluation of this study. The
alveolar bone (acute alveolar abscess) and, in theclinical efficacy of an antimicrobial treatment is
worst cases, it can evolve to osteomyelitis. In otherdetermined by its pharmacokinetic and pharmaco-
cases, the chronic irritation from the necrotic pulpdynamic profile at the infection site. There are no
may result in periapical granuloma or cyst forma-data in the literature about pharmacokinetic profiles
tion, which may be relatively asymptomatic. antimi-of antimicrobials in the gingival tissue and, there-
crobial therapy is indicated when infection has per-fore, it is not possible to establish pharmacokinetic/
forated the cortex and has spread into the surround-pharmacodynamic parameters using concentration
ing soft tissue. When the bone is affected,data from infected tissues. However, there are some
amoxicillin/clavulanic acid, clindamycin, me-data about drug penetration onto the gingival tissue
tronidazole or fluoroquinolones (levofloxacin) areand the periodontal pocket, which may be useful.recommended. As metronidazole and fluoroqui-For example, azithromycin,[63,64] clindamycin,[65]
© 2005 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2005; 44 (3)

8/19/2019 FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf
http://slidepdf.com/reader/full/farmacocineticaydinamicadelosatbpdf 10/12
314 Isla et al.
nolones have shown good bone penetration,[71,72] a formance of clinical trials is necessary to confirm
combined therapy is recommended in these cases; the usefulness of this methodology.
amoxicillin/clavulanic acid will be a good option forpathogens sited in soft tissues, as we have deter- Acknowledgementsmined in our study, and metronidazole and levoflox-
We would like to thank the Basque Government for theacin will be good options for anaerobes sited in thepre-doctoral research grant to Arantxa Isla. This study wasbone.supported by the Microbiology Unit of Santiago Apostol
Additional studies to establish in vivo efficacy of Hospital and the Laboratory of Pharmacy and Pharmaceutical
different antimicrobials against different pathogens Technology, University of the Basque Country, Vitoria-Gas-
teiz, Spain.in odontogenic infections would be of great interest
to corroborate these results; otherwise, it would be
necessary to modify the pharmacokinetic/pharmaco-Referencesdynamic breakpoints that allow us to predict effica- 1. Ellen RP, McCulloch CA. Evidence versus empiricism: rational
use of systemic antimicrobial agents for treatment of periodon-cy in this kind of pathological process (especiallytitis. Periodontol 2000 1996; 10: 29-44
for antimicrobials that reach different concentra-2. Longman LP, Preston AJ, Martin MV, et al. Endodontics in the
adult patient: the role of antibiotics. J Dent 2000; 28 (8): 539-tions in orofacial tissues than in plasma). Once those48new breakpoints have been established (if necessa-
3. Kuriyama T, Karasawa T, Nakasawa K, et al. Bacteriologicry) by applying the methodology used in our study, features and antimicrobial susceptibility in isolates from
orofacial odontogenic infections. Oral Surg Oral Med Oralwe would have a more realistic prediction of thePathol Oral Radiol Endod 2000; 90 (5): 600-8
efficacy of the antimicrobial drugs.4. Palmer NOA, Martin MV, Pealing R, et al. Antibiotic prescrib-
ing knowledge of National Health Service general dental prac-
titioners in England and Scotland. J Antimicrob Chemother2001; 47 (2): 233-7Conclusion
5. Jaunay T, Sambrook P, Goss A. Antibiotic prescribing practices
by South Australian general dental practitioners. Aust Dent J
2000; 45 (3): 179-86The study of pharmacokinetic/pharmacodynamic6. Roy K, Bagg J. Antibiotic prescribing by general dental practi-
parameters could be a useful tool in evaluating thetioners in the Greater Glasgow Health Board, Scotland. Br
efficacy of different antimicrobial treatments in end- Dent J 2000; 188 (12): 674-6
7. Dupon M, Cohere-Moleres MF, Dupon C, et al. Evaluation of odontics, especially considering that there are fewantibiotherapy in dental surgery [in French]. Presse Med 1994;
controlled, double-blind clinical trials that provide 23 (39): 1803-8
8. Yingling NM, Byrne BE, Hartwell GR. Antibiotic use by mem-conclusive evidence of therapeutic benefit[2] and,bers of the American Association of Endodontists in the year
taking that into account, it is very uncommon to2000: report of national survey. J Endod 2002; 28 (5): 396-404obtain microbiological data in clinical practice. 9. Dailey YM, Martin MV. Are antibiotics being used appropriate-
ly for emergency dental treatment? Br Dent J 2001; 191 (7):Applying this methodology, we have observed391-3
that amoxicillin/clavulanic acid and clindamycin are 10. Rehan HS, Singh C, Tripathi CD, et al. Study of drug utilization
pattern in dental OPD at tertiary care teaching hospital. Indianthe only orally administered antimicrobials that al-J Dent Res 2001; 12 (1): 51-6
low us to obtain adequate pharmacokinetic/pharma-11. Gaspar L, Vago P. The tendency of antibiotic therapy in dental
and oral surgical practice [in Hungarian]. Fogorv Sz 1998; 91codynamic parameters against the most commonly(3): 67-78isolated oral pathogens for the treatment of orofacial
12. Schentag JJ, Swanson DJ, Smith IL. Dual individualization:infections. Nevertheless, the use of drug concentra- antibiotic dosage calculation from the integration of in vitro
pharmacodynamics and in vivo pharmacokinetics. J An-tion measurements in orofacial tissues would allowtimicrob Chemother 1985; 15 Suppl. A: 47-57
us to obtain better efficacy indices than those with 13. Sanchez Navarro A, Sanchez Recio MM. Basis of anti-infective
plasma concentration data. Furthermore, the per- therapy: pharmacokinetic-pharmacodynamic criteria and
© 2005 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2005; 44 (3)

8/19/2019 FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf
http://slidepdf.com/reader/full/farmacocineticaydinamicadelosatbpdf 11/12
PK/PD of Antimicrobials in Odontogenic Infections 315
methodology for dual dosage individualisation. Clin over a 3 day period in healthy volunteers. J Antimicrob
Pharmacokinet 1999; 37 (4): 289-304 Chemother 2001; 47 (1): 61-6
29. Ballow CH, Amsden GW, Highet VS, et al. Pharmacokinetics of 14. Schentag JJ. Antimicrobial action and pharmacokinetics/phar-
oral azithromycin in serum, urine, polymorphonuclear leuco-macodynamics: the use of AUIC to improve efficacy and avoidcytes and inflammatory vs non-inflammatory skin blisters inresistance. J Chemother 1999; 11 (6): 426-39
healthy volunteers. Clin Drug Invest 1998; 15 (2): 159-6715. Andes D. Pharmacokinetic and pharmacodynamic properties of
30. Chien SC, Rogge MC, Gisclon LG, et al. Pharmacokineticantimicrobials in the therapy of respiratory tract infections.
profile of levofloxacin following once-daily 500 milligramCurr Opin Infect Dis 2001; 14 (2): 165-72
oral or intravenous doses. Antimicrob Agents Chemother16. Ebert SC. Pharmacokinetic-pharmacodynamic modeling of irre-1997; 41 (10): 2256-60versible drug effects. In: Derendorf H, Hochhaus G, editors.
31. Chien SC, Wong FA, Fowler CL, et al. Double-blind evaluationHandbook of pharmacokinetic/pharmacodynamic correlation.
of the safety and pharmacokinetics of multiple oral once-dailyNew York: CRC Press, 1995: 35-56
750-milligram and 1-gram doses of levofloxacin in healthy17. Li RC, Zhu M, Schentag JJ. Achieving an optimal outcome involunteers. Antimicrob Agents Chemother 1998; 42 (4): 885-8the treatment of infections: the role of clinical pharmacokinet-
32. Dan M, Yampolsky E, Poch F. Serum concentrations and ex ics and pharmacodynamics of antimicrobials. Clin
vivo inhibitory/bactericidal activity of clindamycin after ad-Pharmacokinet 1999; 37 (1): 1-6
ministration of two oral dosages. Chemotherapy 1997; 43 (4):18. MacGowan AP, Bowker KE. Continuous infusion of β-lactam227-31antibiotics. Clin Pharmacokinet 1998; 35 (5): 391-402
33. Deppermann KM, Lode H, Hoffken G, et al. Influence of 19. Periti P, Mazzei T. Clarithromycin: pharmacokinetic and phar-ranitidine, pirenzepine, and aluminum magnesium hydroxidemacodynamic interrelationships and dosage regimen. Jon the bioavailability of various antibiotics, including amox-Chemother 1999; 11 (1): 11-27icillin, cephalexin, doxycycline, and amoxicillin-clavulanic
20. Loza E, Morosini MI, Negri MC, et al. Estudio multicentricoacid. Antimicrob Agents Chemother 1989; 33 (11): 1901-7
nacional de la actividad in vitro de moxifloxacino frente a34. Dunn CJ, Barradell LB. Azithromycin: a review of its pharma-patogenos respiratorios. Rev Esp Quimioter 2000; 13 (1): 37-
cological properties and use as 3-day therapy in respiratory43tract infections. Drugs 1996; 51 (3): 483-505
21. Roche Y, Yoshimori RN. In vitro activity of spiramycin and35. Ernst ME, Ernst EJ, Klepser ME. Levofloxacin and trovaflox-metronidazole alone or in combination against clinical isolates
acin: the next generation of fluoroquinolones? Am J Healthfrom odontogenic abscesses. J Antimicrob Chemother 1997;Syst Pharm 1997; 54: (22): 2569-8440 (3): 353-7
36. Fish DN, Chow AT. The clinical pharmacokinetics of levoflox-22. Hillier SL, Moncla BJ. Peptostreptococcus, Propionibacterium,acin. Clin Pharmacokinet 1997; 32 (2): 101-19 Eubacterium, and other non-sporeforming anaerobic gram-
37. Fraschini F, Scaglione F, Falchi M, et al. Pharmacokinetics andpositive bacteria. In: Murray PR, Baron EJ, Pfaller MA, et al.,tissue distribution of amoxicillin plus clavulanic acid after oraleditors. Manual of clinical microbiology. 6th ed. Washington,administration in man. J Chemother 1990; 2 (3): 171-7DC: ASM Press, 1995: 587-602
38. Frydman AM, Le Roux Y, Desnottes JF, et al. Pharmacokinetics23. Woodcock JM, Andrews JM, Boswell FJ, et al. In vitro activityof spiramycin in man. J Antimicrob Chemother 1988; 22of BAY 12-8039, a new fluoroquinolone. Antimicrob AgentsSuppl. B: 93-103Chemother 1997; 41 (1): 101-6
39. Gatti G, Flaherty J, Bubp J, et al. Comparative study of bioavai-24. Kuriyama T, Karasawa T, Nakasawa K, et al. Bacteriology andlabilities and pharmacokinetics of clindamycin in healthy vol-antimicrobial susceptibility of gram-positive cocci isolatedunteers and patients with AIDS. Antimicrob Agentsfrom pus specimens of orofacial odontogenic infections. OralChemother 1993; 37 (5): 1137-43Microbiol Immunol 2002; 17 (2): 132-5
40. Ishii K, Saito Y, Itai S, et al. Comparative study of 25. Matto J, Asikainen S, Vaisanen ML, et al. Beta-lactamasepharmacokinetic parameters between clarithromycin andproduction in Prevotella intermedia, Prevotella nigrescens,erythromycin stearate in relation to their physicochemicaland Prevotella pallens genotypes and in vitro susceptibilitiesproperties. Drug Dev Ind Pharm 1998; 24 (2): 129-37to select antimicrobial agents. Antimicrob Agents Chemother
1999; 43 (10): 2383-8 41. Jetlund O, Thurmann-Nielsen E, Walstad RA. Comparison of
the serum and tissue concentrations of cefuroxime from26. Appelbaum PC, Spangler SK, Jacobs MR. β-lactamase produc-cefuroxime axetil and phenoxymethylpenicillin in patients un-tion and susceptibilities to amoxicillin, amoxicillin-dergoing tonsillectomy. Int J Clin Pharmacol Res 1991; 11 (1):clavunanate, ticarcillin, ticarcillin-clavulanate, cefoxitin,1-6imipenem, and metronidazole of 320 non- Bacteroides fragilis
Bacteroides isolates and 129 fusobacteria from 28 US centres. 42. Klotz U. Pharmacokinetic considerations in the eradication of
Antimicrob Agents Chemother 1990; 34 (8): 1546-50 Helicobacter pylori. Clin Pharmacokinet 2000; 38 (3): 243-70
27. Sbordone L, Barone A, Ramaglia L, et al. Antimicrobial suscep- 43. Lalak NJ, Morris DL. Azithromycin clinical pharmacokinetics.
tibility of periodontophatic bacteria associated with failing Clin Pharmacokinet 1993; 25 (5): 370-4
implants. J Periodontol 1995; 66 (1): 69-74 44. Lang CC, Moreland TA, Davey PG. Bioavailability of cefurox-
28. Amsden GW, Gray CL. Serum and WBC pharmacokinetics of ime axetil: comparison of standard and abbreviated methods. J
1500mg of azithromycin when given either as a single dose or Antimicrob Chemother 1990; 25 (4): 645-50
© 2005 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2005; 44 (3)

8/19/2019 FARMACOCINETICA_Y_DINAMICA_DE_LOS_ATB.pdf
http://slidepdf.com/reader/full/farmacocineticaydinamicadelosatbpdf 12/12
316 Isla et al.
45. Liu CM, Chen YK, Yang TH, et al. High-performance liquid 61. National Committee for Clinical Laboratory Standards. Meth-
chromatographic determination of clindamycin in human plas- ods for antimicrobial susceptibility testing of anaerobic bacte-ma or serum: application to the bioequivalency study of
ria: approved standard. 5th ed. Wayne (PA): National Commit-
clindamycin phosphate injections. J Chromatogr B 1997; 696 tee for Clinical Laboratory Standards, 2000. Document M11-(2): 298-302A4; 21 (2)
46. Macdonald H, Kelly RG, Allen ES, et al. Pharmacokinetic62. National Committee for Clinical Laboratory Standards. Meth-studies on minocycline in man. Clin Pharmacol Ther 1973; 14
ods for dilution antimicrobial susceptibility tests for bacteria(5): 852-61
that grow aerobically: approved standard. 5th ed. Wayne (PA):47. Mensa J, Gatell JM, Jimenez de Anta MT, et al. Guia de
National Committee for Clinical Laboratory Standards, 2000.terapeutica antimicrobiana. 12th ed. Barcelona: Masson SA,
2001 Document M7-A5
63. Malizia T, Tejada MR, Ghelardi E, et al. Periodontal tissue48. Miglioli PA, Pivetta P, Strazzabosco M, et al. Effect of age on
single- and multiple-dose pharmacokinetics of erythromycin. disposition of azithromycin. J Periodontol 1997; 68 (12):
Eur J Clin Pharmacol 1990; 39 (2): 161-4 1206-9
49. Montoya MA, Girard ME, Torres S, et al. Relative bioavailabili-64. Blandizzi C, Malizia T, Lupetti A, et al. Periodontal tissuety among metronidazole tablets [in Spanish]. Gac Med Mex disposition of azithromycin in patients affected by chronic
1988; 124 (1-2): 19-25inflammatory periodontal diseases. J Periodontol 1999; 70 (9):
50. Nix DE, Symonds WT, Hyatt JM, et al. Comparative 960-6pharmacokinetics of oral ceftibuten, cefixime, cefaclor and
65. Calatayud J, Martinez-Sicilia A, Lucas M. Revision de lacefuroxime axetil in healthy volunteers. Pharmacotherapy
clindamicina. Av Odontoestomatol 1988; 8: 397-4021997; 17 (1): 121-5
66. Denks A, Plagmann HC, Lange DE. Concentration and determi-51. Overbosch D, Mattie H, van Furth R. Comparative pharmacody-nation of spiramycin in gingiva and saliva [in German]. Dtschnamics and clinical pharmacokinetics of phenoxymethylpeni-
cillin and pheneticillin. Br J Clin Pharmacol 1985; 19 (5): 657- Zahnarztl Z 1972; 27 (4): 336-40
6867. Ciancio SG, Mather ML, McMullen JA. An evaluation of mino-
52. Plaisance KI, Drusano GL, Forrest A, et al. Pharmacokinetic cycline in patients with periodontal disease. J Periodontol
evaluation of two dosage regimens of clindamycin phosphate. 1980; 51 (9): 530-4Antimicrob Agents Chemother 1989; 33 (5): 618-20
68. Van Oosten MA, Notten FJ, Mikx FH. Metronidazole concen-53. Quiding H, Arwidsson HG, Grahn Hakansson EG, et al. Saliva-
trations in human plasma, saliva and gingival crevice fluidresistant coating of tablets prevents oral release of penicillin:
after a single dose. J Dent Res 1986; 65 (12): 1420-3plasma but not saliva equivalence. Eur J Clin Pharmacol 1998;
54 (9-10): 749-52 69. Britt MR, Pohlod DJ. Serum and crevicular concentrations after
a single oral dose of metronidazole. J Periodontol 1986; 57 (2):54. Reed M. Clinical pharmacokinetics of amoxicillin and clavu-104-7lanate. Pediatr Infect Dis J 1996; 15 (10): 949-54
70. Sefton AM, Maskell JP, Beighton D, et al. Azithromycin in the55. Siegmund W, Zschiesche M, Franke G, et al. Bioavailability of
treatment of periodontal disease: effect on microbial flora. Jmetronidazole formulations (Vagimid®). Pharmazie 1992; 47
(7): 522-5 Clin Periodontol 1996; 23: 998-1003
71. Gattis WA. A selected review of antimicrobial concentrations56. Saivin S, Houin G. Clinical pharmacokinetics of doxycyclineand minocycline. Clin Pharmacokinet 1988; 15 (6): 355-66 within tissues of the bone, eye, and lung. Antimicrob Infect Dis
Newslett 1994; 13: 75-8657. Trampuz A, Wenk M, Rajacic Z, et al. Pharmacokinetics and
pharmacodynamics of levofloxacin against Streptococcus 72. Prieto J, Gomez-Lus ML. Tratamiento de las infecciones pneumoniae and Staphylococcus aureus in human skin blister
bucodentarioas. In: Dronbic L, editor. Tratamiento an-fluid. Antimicrob Agents Chemother 2000; 44 (5): 1352-5
timicrobiano. Madrid: Ergon, 2002: 497-50358. Turnidge J. Pharmacokinetics and pharmacodynamics of fluoro-
quinolones. Drugs 1999; 58 Suppl. 2: 29-36
Correspondence and offprints: Dr Jose Luis Pedraz,59. Wise R, Bennet SA, Dent J. The pharmacokinetics of orally
absorbed cefuroxime compared with amoxycillin/clavulanic Laboratorio de Farmacia y Tecnologia Farmaceutica,acid. J Antimicrob Chemother 1984; 13 (6): 603-10
Facultad de Farmacia, Paseo de la Universidad nº 7. 01006,60. Jacobs MR. Optimisation of antimicrobial therapy using
Vitoria-Gasteiz, Spain.pharmacokinetic and pharmacodynamic parameters. Clin
Microbiol Infect 2001; 7 (11): 589-96 E-mail: [email protected]
© 2005 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2005; 44 (3)