El Aerobic Mejora El Sueño 5
-
Upload
marcoscasas -
Category
Documents
-
view
219 -
download
0
Transcript of El Aerobic Mejora El Sueño 5
-
8/12/2019 El Aerobic Mejora El Sueo 5
1/20
Jointly sponsored by Postgraduate Institute for Medicineand MedEdicus LLC
is activity is supported by an educational grant from Merck & Co.
New DirectionsManagement ofin the
Balancing
TerapeuticsandPathophysiology
Proceedings From an Expert Roundtable Discussion
Insomnia
Release date: October 10, 2013
Expiration date: October 31, 2014Estimated time to complete activity: 1.5 hours
Distributed with
-
8/12/2019 El Aerobic Mejora El Sueo 5
2/20
Target Audienceis activity has been designed to meet the educational needsof physicians involved in the management of patients withinsomnia disorder.
Statement of Need/Program OverviewAn estimated 40 to 70 million Americans are affected byinsomnia. According to these estimates, twice as many Americansuffer from insomnia than from major depression. However, the
true prevalence of insomnia is unknown because it isunderdiagnosed and underreported. Recent updates in thenosology and diagnostic criteria for insomnia have occurred aswell as advances in understanding pathophysiology, which, inturn, has led to the development of potential new treatments.e burden of medical, psychiatric, interpersonal, and societalconsequences that can be aributed to insomnia and theprevalence of patients with insomnia disorder treated in primarycare underscore the importance of continuing medical educatio(CME) that improves the clinical understanding, diagnosis, andtreatment of the disorder by primary care providers. iscontinuing education activity is based on an expert roundtable
discussion and literature review and provides an update ininsomnia disorder.
Educational ObjectivesAer completing this activity, the participant should be beerable to:
Perform a rapid assessment that leads to a diagnosis ofinsomnia disorder
Summarize the proposed pathophysiology ofinsomnia disorder
Evaluate current and emerging nonpharmacologic andpharmacologic therapies for insomnia disorder
Appropriately select therapy for individual patients
with insomnia disorder
Accreditation Statementis activity has been planned and implemented in accordancewith the Essential Areas and policies of the Accreditation Councfor Continuing Medical Education through the joint sponsorshiof Postgraduate Institute for Medicine and MedEdicus LLC. ePostgraduate Institute for Medicine is accredited by the ACCMEto provide continuing medical education for physicians.
Credit Designatione Postgraduate Institute for Medicine designates this endurinmaterial for a maximum of 1.5AMA P Category 1 Credit(s).
Physicians should claim only the credit commensurate with theextent of their participation in the activity.
Disclosure of Conicts of InterestPostgraduate Institute for Medicine (PIM) requires instructors,planners, managers, and other individuals who are in a position control the content of this activity to disclose any real or apparenconict of interest (COI) they may have as related to the contenof this activity. All identied COI are thoroughly veed andresolved according to PIM policy. PIM is commied to providinits learners with high quality CME activities and related materiathat promote improvements or quality in healthcare and not aspecic proprietary business interest of a commercial interest.
2
Larry Culpepper, MD, MPHCo-ChairProfessor and Chairman of Family Medicine
Boston University School of Medicine
Boston University Medical Center
Boston, Massachuses
Tom Roth, PhDCo-ChairDirector of Research
Sleep Disorders and Research Center
Henry Ford Hospital
Detroit, Michigan
Sonia Ancoli-Israel, PhDProfessor Emeritus of Psychiatry and Medicine
Professor of Research
University of California, San Diego
La Jolla, California
Andrew Krystal, MDDirector, Insomnia and Sleep Research Program
Professor of Psychiatry and Behavioral Sciences
Duke University Medical Center
Durham, North Carolina
Phyllis Zee, MD, PhDBenjamin and Virginia T. Boshes Professor in Neurology
Director, Sleep Disorders Center
Northwestern University
Chicago, Illinois
Faculty
-
8/12/2019 El Aerobic Mejora El Sueo 5
3/20
Faculty Disclosuresefaculty reported the following nancial relationships orrelationships to products or devices they or their spouse/lifepartner have with commercial interests related to the content ofthis CME activity:
Sonia Ancoli-Israel, PhD, had a nancial agreement or affiliationduring the past year with the following commercial interests inthe form of Consultant Fees: Ferring Pharmaceuticals; Merck &Co.; and Prudue Pharma L.P.
Larry Culpepper, MD, MPH, had a nancial agreement oraffiliation during the past year with the following commercialinterests in the form of Consultant Fees: Boehringer IngelheimPharmaceuticals Inc.; Forest Labs; Janssen Pharmaceuticals, Inc.;Jazz Pharmaceuticals plc; H. Lundbeck A/S; Merck & Co.;Pzer Inc.; Recki Benckiser Pharmaceuticals Inc.; SunovionPharmaceuticals Inc.; and Takeda Pharmaceuticals Inc.Speakers Bureau: Merck & Co. Ownership Interest: M3(My Mood Monitor).
Andrew Krystal, MD, had a nancial agreement or affiliationduring the past year with the following commercial interests in
the form of Consultant Fees:Abbo Laboratories; AstraZeneca;Bristol-Myers Squibb; Eisai Inc.; Jazz Pharmaceuticals plc;Johnson & Johnson; Merck & Co.; Neurocrine Biosciences, Inc.;Novartis; Respironics, Inc.; Roche; Sunovion PharmaceuticalsInc.; and Teva Pharmaceutical Industries Ltd. ContractedResearch:Abbo Laboratories; Astellas Pharma; Brainsway;National Institutes of Health; NeoSynch; Pzer Inc.; St. JudeMedical (for Advanced Neuromodulation Systems [ANS]); andTeva Pharmaceutical Industries Ltd.
Tom Roth, PhD, had a nancial agreement or affiliation duringthe past year with the following commercial interests in the formof Consultant Fees:Jazz Pharmaceuticals plc; Merck & Co.;
Neurocrine Biosciences, Inc.; Novartis; Pzer Inc.; PurduePharma L.P.; Speakers Bureau: Purdue Pharma L.P. ContractedResearch: Impax Laboratories, Inc.; Valeant Pharmaceuticals(for CeraVe).
Phyllis C. Zee, MD, PhD, had a nancial agreement or affiliationduring the past year with the following commercial interests inthe form of Consultant Fees: Ferring Pharmaceuticals; JazzPharmaceuticals plc; Merck & Co.; Purdue Pharma L.P.; TakedaPharmaceuticals Inc.; Vanda Pharmaceuticals Inc.; and UCB, Inc.Contracted Research: Philips Respironics. Ownership Interest: TevaPharmaceutical Industries Ltd.
eplanners and managers reported the following nancial
relationships or relationships to products or devices they or theirspouse/life partner have with commercial interests related to thecontent of this CME activity:
e following PIM planners and managers, Laura Excell, ND,NP, MS, MA, LPC, NCC, Trace Hutchison, PharmD, Samantha
Maiucci, PharmD, CCMEP, andJan Schultz, RN, MSN,CCMEP, and the following MedEdicus editors and planners,Casey Covre, PharmD, BCPS, and Cynthia Tornallyay, RD,
MBA, CCMEP, hereby state that they or their spouse/life partnerdo not have any nancial relationships or relationships toproducts or devices with any commercial interest related to thecontent of this activity of any amount during the past 12 months.
Method of Participation and Request for Creditere are no fees for participating and receiving CME credit forthis activity. During the period October 10, 2013, throughOctober 31, 2014, participants must read the learning objectivesand faculty disclosures and study the educational activity.
PIM supports Green CME by offering your Request for Creditonline. If you wish to receive acknowledgment for completing thisactivity, please complete the post-test and evaluation on
www.cmeuniversity.com. On the navigation menu, click onFind Post-test/Evaluation by Course and search by course ID9496. Upon registering and successfully completing the post-testwith a score of 70% or beer and the activity evaluation, yourcerticate will be made available immediately.
Media
Monograph
Disclosure of Unlabeled Useis educational activity may contain discussion of publishedand/or investigational uses of agents that are not indicated by theFDA. e planners of this activity do not recommend the use ofany agent outside of the labeled indications.
e opinions expressed in the educational activity are those of thefaculty and do not necessarily represent the views of the planners.Please refer to the official prescribing information for eachproduct for discussion of approved indications, contraindications,and warnings.
DisclaimerParticipants have an implied responsibility to use the newlyacquired information to enhance patient outcomes and theirown professional development. e information presented inthis activity is not meant to serve as a guideline for patientmanagement. Any procedures, medications, or other courses
of diagnosis or treatment discussed or suggested in this activityshould not be used by clinicians without evaluation of theirpatients conditions and possible contraindications and/ordangers in use, review of any applicable manufacturers productinformation, and comparison with recommendations ofother authorities.
-
8/12/2019 El Aerobic Mejora El Sueo 5
4/20
4
IntroductionAn estimated 40 to 70 million Americans have insomnia.1
According to these estimates, twice as many Americans suffer ominsomnia than om major depression.2Patients with insomniaequently report physical and emotional health problems,compromised social functioning, and daytime distress. Commonrisk factors for insomnia include female gender, advanced age,
comorbid disease, and occupations involving shi work.Importantly, comorbid medical disorders are becoming moreappreciated as risk factors for insomnia.
Work productivity is negatively impacted by insomnia. In the 2009US Workers America Insomnia Survey, presenteeism (low on-the-jobwork performance dened in the metric of lost workday equivalents)accounted for nearly 8 days of annual lost work performance perworker, equating to $2280 in individual-level human capital value.When extrapolated to the entire US workforce over the course of ayear, insomnia causes 252.7 million days of lost work performance,resulting in a loss of $63.2 billion.3
e magnitude of insomnia-related problems has spurred research,resulting in an improved understanding of the disorder. Over thepast decade, several changes have been made with regard to thenosology of insomnia, most notably the recent realization thatinsomnia is a disorder. In the past, insomnia was thought to besecondary to another medical condition. e Diagnostic andStatistical Manual of Mental Disorders, Fih Edition (DSM-5),has recently renamed the diagnosis as insomnia disorder,emphasizing that insomnia is a disorder in its own right eventhough it typically coexists with other comorbid medicalconditions, including depression, anxiety, chronic pain, andcardiovascular diseases.4In addition, the Diagnostic andStatistical Manual of Mental Disorders, Fourth Edition, Text
Revision, diagnostic criteria have been updated in the DSM-5 toinclude more stringent measures regarding the chronicity ofinsomnia-related symptoms. For the purpose of this monograph,the term insomnia will be used as a disorder that meets theDSM-5 criteria, which include the following: (1) difficulty fallingand/or staying asleep; (2) the sleep difficulty is accompanied bynext-day symptoms of distress/impairment; (3) sleep-relatedsymptoms occur at least 3 times per week for a minimum of3 months; and (4) symptoms persist despite adequateopportunities and circumstances to sleep.4
Insomnia is a prevalent and costly public health concern that isassociated with signicant long-term effects on physical,
psychological, and occupational functioning. In order to minimizethe societal impact of insomnia and the burden it creates on thehealthcare system, families, and patients, clinicians need toimprove their recognition and treatment of insomnia as well ascoexisting medical conditions. is approach starts with having aninitial discussion with patients regarding the quality of their sleep.
Despite its prevalence, insomnia remains undertreated andunderreported. Patients are reluctant to seek medical treatment,and sleep is not commonly discussed during office visits. iscontinuing medical education/continuing education (CME/CE)activity is designed to update readers on the pathophysiology ofinsomnia, the interrelationships of insomnia and comorbiddisease, and new directions in the management of insomnia.
Pathophysiology of InsomniaCurrent research suggests that insomnia is a disorder ofhyperarousal that is present 24 hours each day. epathophysiology of insomnia is multifactorial and may be thoughof in terms of dysregulation involving the following 3 componentneurophysiologic hyperactivation of the sympathetic nervoussystem; neuroendocrine dysregulation of hormones associated witarousal; and cognitive/behavioral responses directed toward sleep
that perpetuate arousal. Expert insights on the pathophysiology ofinsomnia from the roundtable discussion will be presented. Figurepresents a schematic diagram of the 24-hour sleep-wake cycle.5
Dr Tom Roth: For years we had this idea that insomnia is anabnormality of the sleep system. Increasingly, we have learned thinsomnia is not an abnormality of the sleep system, but it is anabnormality of the wake/arousal system. Over a decade ago, Sapand colleagues proposed the ip-op switch model of sleep-wakregulation,6which contains 2 sets of mutually inhibitory neuralelements: wake-promoting inuences on 1 side and sleep-promotiinuences on the other. e monoaminergic nuclei (MN) are amajor inuence of the wake-promoting system, and sleep is
inuenced by the ventrolateral preoptic nucleus (VLPO), which isgroup of cells that generate non-rapid eye movement (NREM) andrapid eye movement (REM) stages of sleep (Figure 2).5 In patientswith normal sleep, the ip-op switch makes sudden transitionsbetween sleep and wakefulness, which explains why a limitedamount of time is spent in these transitional states throughout thecourse of a 24-hour day (Figure 3).6 In patients with insomnia,however, their ability to turn off the wake-promoting inuences ofthe ip-op switch is weakened, resulting in extended periods oftime in transitional states and a prolonged state of wake.
Dr Andrew Krystal: ere are a number of objective measures thasupport this model of hyperarousal, including elevations in heartrate and heart rate variability. For example, Bonnet and Arandperformed a 36-hour study that showed the heart rate increased an
the mean heart rate variability decreased in all stages of sleep in thgroup of people with insomnia compared to the control group ofpeople who have normal sleep.7 Studies have also found thatpatients with insomnia, when compared to controls, have highermetabolic rates throughout the course of a 24-hour day, furthersuggesting arousal in the wake-promoting regions in the brain.8
Dr Larry Culpepper: ere appears to be a neuroendocrinecomponent to this condition as well. Vgontzas and colleaguesfound that levels of adrenocorticotropic hormone and cortisolwere signicantly elevated in patients with insomnia compared tmatched controls, which results in increased arousal andassociated sleeplessness. In addition, patients with a higher degrof sleep disturbance secreted more cortisol compared to thosewith less sleep disturbance.9
For years we had this idea that insomnia is
an abnormality of the sleep system. Increasingly, whave learned that insomnia is not an abnormalityof the sleep system, but it is an abnormality of the
wake/arousal system. Dr Tom Roth
-
8/12/2019 El Aerobic Mejora El Sueo 5
5/20
Dr Andrew Krystal: Positron emission tomography has shown
that patients with insomnia exhibit greater brain glucosemetabolism during sleep and wake periods compared to peoplewho have normal sleep, indicating the inability of patients withinsomnia to appropriately transition from wake to sleep.10 Table 1lists elevated physiologic factors that have been observed inpatients who have insomnia, which are suggestive of hyperarousal.
Dr Phyllis Zee: Stepanski and colleagues comparedpolysomnography and multiple sleep latency test data frompatients seeking evaluation for chronic insomnia with data from
patients without sleep problems.11 e insomnia group sleptsignicantly less than the control group, yet they weresignicantly less sleepy the next day compared with matchedcontrols. is study found that if given the chance to sleep duringthe day, patients with insomnia take longer than the generalpopulation to fall asleep. Insomnia is a 24-hour disorder ofhyperarousal associated with difficulty sleeping at any time of day.
Dr Sonia Ancoli-Israel: is inability to sleep during the dayhighlights why the initial assessment of sleep-related symptomsis so important. If patients indicate theyre having difficultysleeping at night but they sleep well during the day, it is lesslikely to be insomnia. Someone with insomnia has difficultyfalling asleep during the day as much as they do at night.
Dr Phyllis Zee: ere are primarily 3 different ways to promotewakefulness: (1) blocking the sleep promoting neurons in theVLPO; (2) exciting the monoaminergic nuclei associated withthe wake system; and (3) stimulation of the orexin neurons.
Dr Tom Roth: I think all of you bring up a great point. When
patients with insomnia get out of bed at 7 oclock in the morning,their insomnia has not gone away. For patients who have
Someone with insomnia has difficultyfalling asleep during the day as much as theydo at night. Dr Sonia Ancoli-Israel
Figure 2.A schematic of the sleep-promoting and wake-promoting areas of the
human brain. ere are multiple cell groups in the brain that contribute to thesleep-wake system. e monoaminergic nuclei (MN) are responsible for promotingwakefulness, while the ventrolateral preoptic nucleus (VLPO) promote sleep.Monoaminergic nuclei of the arousal pathway include noradrenergic, serotonergic,dopaminergic, and histaminergic neurons located in the pedunculopontine andlaterodorsal tegmental nucleus (PPT/LDT), locus coeruleus (LC), dorsal andmedian raphe nucleus (RN), and tuberomammillary nucleus (TMN), respectively.Every 24 hours the arousal system is overtaken by inhibitory neurons of the VLPO,resulting in the transition from wakefulness to sleep.
Table 1. Physiologic Factors Increased During Sleep in PatientsWith Insomnia
Body temperature
Brain glucose metabolism
Resting heart rate
Cortisol level
Electroencephalogram beta wave activity
Insomnia is a 24-hour disorder ofhyperarousal associated with difficulty sleeping
at any time of day.Dr Phyllis Zee
Hour 0 Hour 24
Wake ~ 16 hrs
2/3 of Sleep-Wake Cycle
Sleep~ 8 hrs
1/3 of Sleep-Wake Cycle
NREM REM
Figure 1.A schematic diagram of the sleep-wake cycle.When transitioning into sleep, an individual begins in non-rapid eye movement (NREM) andremains in this stage for approximately 85 minutes. Aer this initial stage of NREM, the brain switches to rapid eye movement (REM) for approximately5 to 10 minutes before switching back to NREM. is 90-minute paern continues throughout the night, with REM intervals becoming longer andNREM intervals becoming shorter until wakefulness occurs. Disruptions in this dened paern of sleep and wakefulness result in disturbances in sleep.Adapted om Rogers and Holmes, 2012.5
-
8/12/2019 El Aerobic Mejora El Sueo 5
6/20
6
myocardial ischemia, we nd that just because they dont haveangina 24 hours a day doesnt mean their cardiovascular function
is normal all of a sudden. People who have insomnia are notsymptomatic 24 hours a day, 7 days a week. ey have insomnia
24 hours a day that expresses itself periodically. e criteria forinsomnia disorder specify that sleep disturbances must occur atleast 3 days a week for a minimum of 3 months for us to considea diagnosis of insomnia.4
Dr Larry Culpepper:What do we know about the underlyingbrain activity or factors that contribute to this hyperarousal?
Dr Andrew Krystal: I dont think we know all that much about iWe know the wake system is more active during sleep in patientwith insomnia, at least to some degree. Additionally, thepsychopathological and behavioral paerns of sleep appear to pla signicant role in some patients with sleep problems. Forexample, when people experience multiple nights of bad sleep anfrustration within their sleeping environment, they begin todevelop the expectation of poor sleep. is expectation becomeperpetuating factor that creates stress and increased activity of thsympathetic nervous system. In addition to the neuroendocrineand physiologic components of hyperarousal, there appears to ba behavioral/psychopathological element to this condition.
Updates in the Diagnostic Criteria andNosology of Insomniae diagnostic criteria for insomnia have undergone recentchanges with the nalization of the DSM-5, most notably with thchronicity of sleep-related disturbances, which the faculty willdiscuss. In addition, insomnia has been renamed insomnia disordeemphasizing the point that while insomnia typically coexists withother medical conditions, it requires separate clinical aention.Becoming more aware of the numerous comorbid conditionsassociated with insomnia is important and may assist clinicians inbeer recognizing and managing insomnia. e followingdiscussion provides insight into the clinical implications of recent
changes in the diagnostic criteria and the signicance of comorbiconditions associated with insomnia.
Please circle the number that best describes your CURRENT severity level of sleep problem(s).
Please rate this past weeks severity of thefollowing insomnia problems:
None Mild Moderate Severe Very severe
1. Difficulty falling asleep 0 1 2 3 4
2. Difficulty staying asleep 0 1 2 3 4
3. Waking up too early 0 1 2 3 4
Verysatised Satised Moderatelysatised Dissatised Very dissatised
4. How satised/dissatised are you with yourcurrent sleep paern?
0 1 2 3 4
Not at all A lile Somewhat Much Very much
5. How noticeable to others do you think yoursleep problem is in terms of impairing thequality of your life?
0 1 2 3 4
6. How worried/distressed are you about yourcurrent sleep problem?
0 1 2 3 4
7. To what extent do you consider your sleepproblem to interfere with your daily functioning
(mood, concentration, work)?
0 1 2 3 4
Table 2. Insomnia Severity Index13
Scoring: 0-7 No c linically signicant insomnia; 8-14 Sub-threshold insomnia; 15-21 Moderate clinical insomnia; 22-28 Severe clinicalinsomnia.Adapted om Morin et al, 2001.13
Figure 3.A schematic drawing of the ip-op switch model of sleep-wake
regulation. e interaction between the ventrolateral preoptic nucleus (VLPO)and the arousal pathways (Orexin [ORX], locus coeruleus [LC], dorsal and medianraphe nucleus [Raphe], and tuberomammillary nucleus [TMN]) is mutuallyinhibiting, functioning like an on-off (ip-op) switch. is ip-op switch ensuresstability between sleep and wakefulness, which results in normal sleep paerns.Insomnia causes dysregulation of the switch, resulting in irregular transitioningbetween sleep-wake states and fragmented sleep. Reprinted with permission,Saper et al, 2005.6
-
8/12/2019 El Aerobic Mejora El Sueo 5
7/20
Dr Larry Culpepper: In terms of how you dene and diagnose
insomnia, what are some key principles that primary careclinicians should know?
Dr Sonia Ancoli-Israel: I think its important for primary careclinicians to, rst of all, ask their patients about sleep. Researchhas shown that 70% of the clinicians dont ask their patients aboutsleep, and more than 50% of the patients dont talk about it.12
us, the rst step is to determine the overall sleep-wake status ofthe patient. If the patient responds that he or she is experiencingsleep problems, then it takes a lile more in-depth questioningregarding the specic symptoms of insomnia and their frequencyand severity. ere are several questionnairesincluding theInsomnia Severity Index (Table 2)13 and the Epworth Sleepiness
Scalethat clinicians can use to facilitate sleep-related discussionwith their patients.
Dr Tom Roth: I think its also important for clinicians to
differentiate sleep disturbance from insomnia because they arenot the same thing. W hen there are inadequate opportunities orcircumstances to sleep, sleep disturbances typically occur. Butthat is not insomnia. An insomnia diagnosis is made when apatient meets the following 4 criteria (Table 3): (1) nighimesymptoms of difficulty falling asleep and/or staying asleep;(2) next-day symptoms of distress/impairment; (3) symptomsoccur at least 3 times per week for a minimum of 3 months; and(4) symptoms persist despite adequate opportunity andcircumstances to sleep.4
Comorbid Conditions Associated
With InsomniaDr Phyllis Zee: I would add that insomnia is now listed asinsomnia disorderin the DSM-5 and the InternationalClassication of Sleep Disorders, ird Edition (ICSD-3)diagnostic manuals. In the past, insomnia was labeled as primary(the absence of an adjunct comorbid condition) or secondary(insomnia arising in the context of another disorder). Althoughinsomnia is oen associated with other conditions, such as pain,depression, anxiety, and cardiovascular diseases, insomnia is itsown distinct disorder (Table 4).14
Table 3. DSM-5 Insomnia Disorder Criteria 780.52 (G47.00)
Note:Acute and short-term insomnia (i.e., symptoms lasting less than 3 monthsbut otherwise meeting all criteria with regard to frequency, intensity, distress,and/or impairment) should be coded as other specied insomnia disorder.
Reprinted with permission om the Diagnostic and Statistical Manual of MentalDisorders, Fih Edition, (Copyright 2013). American Psychiatric Association.All Rights Reserved.
A. A predominant complaint of dissatisfaction with sleep quantityor quality, associated with one (or more) of the followingsymptoms:
1. Difficulty initiating sleep. (In children, this may manifest asdifficulty initiating sleep without caregiver intervention.)
2. Difficulty maintaining sleep, characterized by frequentawakenings or problems returning to sleep aer awakenings.(In children, this may manifest as difficulty returning tosleep without caregiver intervention.)
3. Early-morning awakening with inability to return to sleep.
B. e sleep disturbance causes clinically signicant distress orimpairment in social, occupational, educational, academic,behavioral, or other important areas of functioning.
C. e sleep difficulty occurs at least 3 nights per week.
D. e sleep difficulty is present for at least 3 months.
E. e sleep difficulty occurs despite adequate opportunityfor sleep.
F. e insomnia is not beer explained by and does not occurexclusively during the course of another sleep-wake disorder(e.g., narcolepsy, a breathing-related sleep disorder, a circadianrhythm sleep-wake disorder).
G. e insomnia is not aributable to the physiological effects of a
substance (e.g., a drug of abuse, a medication).H. Coexisting mental disorders and medical conditions do not
adequately explain the predominant complaint of insomnia.
Specify if:
With nonsleep disorder mental comorbidity, includingsubstance use disorders
With other medical comorbidity
With other sleep disorder
Coding note: e code 780.52 (G47.00) applies to all threespeciers. Code also the relevant associated mental disorder,medical condition, or other sleep disorder immediately aerthe code for insomnia disorder in order to indicate theassociation.
Specify if:
Episodic: Symptoms last at least 1 month but less than3 months.
Persistent: Symptoms last 3 months or longer.
Recurrent: Two (or more) episodes within the spaceof 1 year.
Comorbid condition
Prevalence of insomnia
In the presenceof comorbid
condition%
In the absence ofcomorbidcondition
%
Cardiovascular disease
Hypertension 26.1 22.8
Heart disease 30.1 23.7
Musculoskeletal disease
Arthritis 30.6 21.5
Back or neck pain 34.2 17.7
Digestive disorders
Diarrhea, constipation, or gas 42.2 20.2
Gastroesophageal reux disease(GERD)
39.2 20.7
Sleep disorders
Sleep apnea 40.9 22.0
Restless leg syndrome 50.6 22.6
Emotional disorders
Major depressive disorder 55.7 21.1
Generalized anxiety disorder 65.6 21.2
Table 4. Prevalence of People With Insomnia and
Comorbid Medical Conditions14
I think its important for primary care clinicians to,rst of all, ask their patients about sleep.
Dr Sonia Ancoli-Israel
-
8/12/2019 El Aerobic Mejora El Sueo 5
8/20
8 Dr Sonia Ancoli-Israel:And since insomnia is its own disorder,you treat it once youve made a diagnosis.
Dr Larry Culpepper: I think what Dr Ancoli-Israel mentioned isthe single most important message to relay to primary careclinicians. In the past, we clinicians have been under the falseimpression that when an existing comorbid condition resolvesfor instance, depressioninsomnia would go away as well. Andthat, quite oen, is not the case.
Dr Tom Roth: If you look at people with depression when theygo into remission, the most common residual symptom isdifficulty sleeping. It is important to understand that the numberof residual symptoms linearly predicts time to relapse ofdepression. e Sequenced Treatment Alternatives to Relieve
Depression (STAR*D) trial described the types and frequency ofresidual depressive symptoms and their relationship todepressive relapse aer treatment with citalopram.15 More than90% of the patients with depression who went into remission hadat least 1 residual depressive symptom, and the most commonresidual symptom domain was sleep-related disturbance(71.7%).15 e study revealed that having a greater number ofresidual symptoms was associated with a higher probability ofrelapse. e point is that treating insomnia enables you to beermanage coexisting disorders.
Dr Andrew Krystal:As mentioned earlier, the error clinicianshave made in the past is undertreating insomnia, expectinginsomnia to get beer once the symptoms of a comorbidcondition improved. Moreover, clinicians should consider thepossibility of underlying comorbid conditions when patientspresent with symptoms suggestive of insomnia. Research showsthat insomnia is a known risk factor for other disorders, mostnotably depression and anxiety. One of the classic studies, theJohns Hopkins Precursors Study, evaluated the associationsbetween self-reported sleep disturbances and subsequent clinicaldepression among medical students (classes 1948-1964; meanfollow-up period of 34 years).16 Patients who reported insomniasymptoms during medical school were twice as likely to developclinical depression compared to those without insomnia
symptoms. Clinicians need to assess whether or not there areunderlying comorbid conditions, such as depression, which maybe intensifying the symptoms of insomnia.
Dr Phyllis Zee: ere is also research to suggest that insomniamay serve as a risk factor of cardiometabolic disease. A recentstudy that evaluated the impact of sleep on levels of fastingglucose, fasting insulin, and estimated insulin resistance showedthat insomnia was associated with a 23% higher fasting glucoselevel and a 48% higher fasting insulin level in patients with type 2diabetes.17 In addition, Vgontzas and colleagues evaluated thejoint effects of insomnia and short sleep duration on diabetesrisk.18 ey showed that patients with insomnia and sleepduration of less than 5 hours were at signicantly higher risk ofdeveloping diabetes compared to people who have normal sleep.
Dr Larry Culpepper: Its also important to remember that thevery treatment of the comorbid condition itself may lead toinsomnia-related symptoms. Respiratory stimulants, selectiveserotonin reuptake inhibitors, beta blockers, and many other druclasses are associated with reports of disturbed sleep (Table 5).1
Differentiating Circadian RhythmDisorders From InsomniaInsomnia is occasionally comorbid with other sleep conditions,including disorders in circadian rhythm. Table 6 lists commoncircadian rhythm sleep disorders (CRSDs) that may occur inconjunction with insomnia20; however, the effective treatmentsfor CRSDs are very different, emphasizing the importance ofdifferentiating sleep-related symptoms of CRSDs from insomnia
Current and Emerging Treatmentfor Insomniae Role of Behavioral Treatment Interventions in
Insomnia Disorder
It is widely accepted that psychological and behavioral factorsplay signicant roles in hyperarousal. Interventions that targetthese factors play an important part in the management ofinsomnia disorder (Table 7).21 Several studies have reported theeffects of behavioral treatment methods administered to patientwith chronic insomnia.22 Patients reported signicant increases isleep time as well as improvements in sleep latency, total waketime, and sleep efficiency aer behavioral interventions. e
Irregular sleep-wake rhythm disorder (ISWD) occurs when a personssleep paern is undened, which typically includes a series of napsthroughout the 24-hour sleep-wake cycle. ISWD is common in elderlypatients with comorbid medical disorders, such as Alzheimers disease.
Delayed sleep phase disorder (DSPD) is a paern of going to bed late inthe evening/early morning and sleeping until late in the aernoon. DSPDis common in teenagers.
Advanced sleep phase disorder (ASPD) is a paern of earlyevening sleepiness and early morning awakening. ASPD is commonin elderly patients.
Shi work disorder occurs when a persons work hours are scheduledduring the normal sleep period.
Non-24-hour sleep disorder occurs when the suprachiasmatic nucleusdoes not receive light from the external environment, resulting in asleep-wake cycle that shis later each day. Non-24-hour disorder iscommon in patients who are totally blind.
Table 6. Circadian Rhythm Sleep Disorders20
And since insomnia is its own disorder, you treat itonce youve made a diagnosis. Dr Sonia Ancoli-Israel
Drug class Medications
Antidepressants Selective serotonin reuptake inhibitors
(uoxetine, citalopram, sertraline, paroxetine),venlafaxine, duloxetine
Decongestants Pseudoephedrine, phenylephrine
Cardiovascular Beta blockers, alpha-receptor antagonists, diuretics
Respiratory eophylline, albuterol
Stimulants Methylphenidate, ephedrine, amphetamines
Opioids Codeine, oxycodone
Table 5. Common Medications at Contribute to Insomnia19
Adapted om Sack et al, 2007.20
-
8/12/2019 El Aerobic Mejora El Sueo 5
9/20
following discussion addresses different types of behavioralinterventions and their impact on insomnia disorder.
Dr Sonia Ancoli-Israel: Before we discuss behavioral therapy, we
should rst discuss Spielman and colleagues 3P model becauseit is the basis of a lot of what we do when administering cognitivebehavioral therapies.23 e key words in the 3P model arepredisposing, precipitating, and perpetuating (Table 8).23
Predisposing factors include conditions such as personality typeor hyperarousal. ese factors predispose patients to sleep-relateddifficulties, but that does not mean they have insomnia. enthere are precipitating factors, such as stress, that may causepatients to lose sleep for a few nights. Geing married, having anew baby, or visiting the in-laws may cause acute sleep-relatedproblems, but those typically resolve on their own aer thetriggering event has disappeared. However, some individuals
experience persistent sleep difficulties, eventually spending moretime in bed in an aempt to get more sleep, which makes theirsleep worse and leads to negative conditioning. ese types ofbehaviors feed into and perpetuate insomnia, making it moredifficult to sleep. Cognitive behavioral therapies target thesenegative learned responses and essentially reteach an individualhow to sleep.
Dr Larry Culpepper: Even a short course of behavioral therapy can
be very effective. In a study involving nurse practitioners trained toprovide behavioral therapy, individuals with chronic insomniaeither received a short course of behavioral therapy, consisting of2 intervention sessions and 2 telephone calls, or they receivedprinted educational materials.24A total of 67% of the individualstreated with behavioral therapy showed a clinical response, comparedto 25% in the control group. In addition, 55% of those in thebehavioral treatment group no longer met the criteria for insomniaat study completion, compared to 13% in the control group.Behavioral therapy is achievable in the primary care seing andcan be performed by a physician or another clinician.
Dr Tom Roth: ere are some data that suggest cognitivebehavioral therapy for insomnia (CBT-I) not only improvesinsomnia symptoms but also augments the remission ofdepression. Manber and colleagues evaluated the addition ofCBT-I to escitalopram (cotherapy) in patients with coexisting
insomnia and depression, compared to escitalopram pluscontrol.25 Cotherapy resulted in a higher rate of remission fromdepression as compared to the control group (61.5% vs 33.3%,respectively) and was associated with a greater rate of remissionfrom insomnia as compared to the control group (50.0% vs 7.7%,respectively). is study emphasizes the point we made earlier:Treating both disorders improves patient outcomes.
Dr Phyllis Zee:We studied the impact of a 16-week aernoonaerobic exercise program plus sleep hygiene measures in patientswith insomnia 55 years and older. e control group consisted ofpatients involved in nonaerobic activity plus sleep hygiene.26 ephysical activity group improved signicantly in sleep quality, sleep
latency, sleep duration, daytime dysfunction, and sleep efficiency.e physical activity group also had signicant reductions indepressive symptoms and daytime sleepiness. Not only doesroutine long-term exercise improve sleep quality in people withinsomnia, but beer sleep the night before predicts your capacityto exercise the next day.
Predisposingfactors
Precipitatingfactors
Perpetuatingfactors
Personality traits Arthritis pain Napping
Genetic traits Psychiatric illness Excessive time in bed
Social factors Stressful event Negative learned behaviors
Table 8. Contributing Factors to Insomnia23
Cognitive behavioral therapies target thesenegative learned responses and essentially reteach
an individual how to sleep. Dr Sonia Ancoli-Israel
Behavioral therapy is achievable in the primarycare seing and can be performed by a physician or
another clinician. Dr Larry Culpepper
Not only does routine long-term exercise improvesleep quality in people with insomnia, but beersleep the night before predicts your capacity to
exercise the next day. Dr Phyllis Zee
Sleep hygiene therapyinvolves teaching healthy lifestyle practices toimprove sleep. Sleep hygiene is recommended to be used in conjunctionwith other cognitive and behavioral therapies. Patients are instructed to(including but not limited to): avoid napping, maintain a regular exerciseprogram and healthy diet, sleep in a quiet, dark environment, and avoidstimulants such as caffeine and nicotine at least 6 hours before bedtime.
Stimulus control therapyis designed to re-associate the bedroom with therapid onset of sleep. Once in bed, if the patient is unable to fall asleep inwhat seems to be about 20 minutes (without looking at a clock), he or sheis instructed to leave the bedroom to engage in a relaxing activity and returnto bed when sleepy (repeat this as necessary). e objective of stimuluscontrol therapy is to limit wake time in bed.Patients should be cautionedabout the possibility of daytime sleepiness during the course of therapy.
Sleep restriction therapylimits time in bed to the amount of time actuallyspent sleeping (normally derived from a sleep log). is approach isdesigned to improve sleep continuity by using sleep restriction to enhancesleep drive (the ability to sleep). Once sleep efficiency improves, theallowed time in bed is gradually increased by 15 to 30 minutes over a periodof several weeks until optimal sleep duration is achieved. e objective ofsleep restriction therapy is to limit wake time in bed.Patients should becautioned about the possibility of daytime sleepiness during the course of therapy.
Relaxation training is a technique that uses muscle relaxation, guidedimagery, and/or abdominal breathing exercises to lower arousal states thatinterfere with sleep.
Cognitive Behavioral erapy for Insomnia (CBT-I) is a combinationof behavioral therapy (eg, sleep restriction, stimulus control) andpsychotherapeutic methods, which involve identifying dysfunctionalbeliefs about sleep and replacing them with more positive alternatives.
Table 7. Common Evidence-Based Cognitive and Behavioral erapiesfor Insomnia21
Adapted om Schue-Rodin et al, 2008.21
-
8/12/2019 El Aerobic Mejora El Sueo 5
10/20
10 Dr Phyllis Zee: Some patients have tried exercising in the lateevening, but that has shown to actually phase shi (delay)circadian rhythms. Not only does exercising late in the eveningenhance symptoms of sympathetic arousal but, at the same time,youre giving the wrong signal to the circadian clock.
Dr Tom Roth: I do not think these insights are unique to sleepmedicine. For example, there are several different methods totreat obesity, but they are all roads to the same outcome. e
exact same thing is true for behavioral therapy. ere is no secretroad to the goal of improving sleep, and it is up to the clinician, hisor her resources, the patients interest, and the patientssophistication as to what the best road to that goal might be.
Prescription MedicationsTable 9 lists medications approved by the US Food and DrugAdministration (FDA) for the treatment of insomnia. ere aremyriad medications that are used to treat insomnia, includingtricyclic antidepressants, antipsychotics, and herbal medications,which have not received regulatory approval for insomnia. Withineach medication class, there are differences in pharmacokinetic/pharmacodynamic indices, which allow clinicians to prescribepatient-specic interventions. Clinicians should consider thefollowing factors when selecting a pharmacologic agent:(1) symptom paerns; (2) comorbid conditions; (3) concurrentmedications; (4) contraindications; (5) side effects; and (6) cost.With the exception of low-dose doxepin, the most recently FDA-approved medications have short half-lives and work during therst few hours of sleep, without signicant sleep maintenanceeffects. In contrast, emerging therapies have longer half-lives andwill presumably have improved effects on sleep maintenance.Expert guidance in the pharmacologic treatment of insomnia andsleep-related disorders wil l be presented.
Dr Andrew Krystal: e older sleep agents are thebenzodiazepines, which potentiate inhibition mediated byGABAAreceptors through binding to a benzodiazepine site on theGABAAreceptor complex. Benzodiazepines work on the sleepside of the ip-op switch. Different subtypes of the GABAAreceptor are located throughout the central nervous system, andbenzodiazepines bind to these receptors without specicity;therefore, not only do they enhance sleep but they also shut downdifferent parts of the brain that we might not want them to,leading to unwanted side effects, including balance and memoryproblems.27 Medications that potentiate GABAAreceptor activityby binding to the benzodiazepine binding site appear to have
some degree of abuse potential, but the abuse seems to be limitedto a subgroup of the population prone to substance abuse.Generally speaking, the majority of people take these medicationsfor therapeutic purposes. Compared to benzodiazepines,nonbenzodiazepines demonstrate greater selectivity in terms ofpreferential binding to a subset of GABAAreceptors, affectingspecic subunits that have regional effects in brain function. Todate, 6 subunits have been identied, and, with the exception ofeszopiclone, the nonbenzodiazepines preferentially bind the alpha1 subunit, which is primarily associated with sedation.28 Becausethe mechanism of action for nonbenzodiazepines is limited to thealpha 1 subunit, they do not appear to relax muscles or provideanxiolysis to the same degree as benzodiazepines.
Dr Tom Roth: A major difference between the classicbenzodiazepines and nonbenzodiazepines relates to
pharmacokinetics. e nonbenzodiazepines tend to have muchshorter half-lives, which typically minimizes next-day sedation.However, female gender and concomitant medications, such asclarithromycin, have been shown to inuence the rate at whichsome of these medications are metabolized.
Dr Andrew Krystal: ere appears to be differences amongagents within the nonbenzodiazepine drug class itself. Whenescitalopram plus zolpidem controlled-release (CR) were
administered to patients with insomnia and comorbid anxiety,sleep-related parameters improved but anxiety scores did not.29
However, when escitalopram plus eszopiclone were administereto a similar patient population, both insomnia and anxiety scoreimproved signicantly. is difference appears to be related to theffects on additional GABAAreceptor subunits, which areassociated with anxiolysis.30 e point is that these medicationsseem to differ clinically, and if you want to help people in terms oinsomnia with comorbid anxiety, eszopiclone is probably a beeadjunctive therapy than zolpidem CR.
Dr Larry Culpepper: Studies have also found that eszopicloneimproves insomnia and depression scores when coadministered
with uoxetine.31 In addition to improvements in sleep parameteat each time point in the study, the eszopiclone cotherapy groupshowed signicantly greater changes in 17-item Hamilton RatingScale for Depression (HAM-D-17) scores, and a signicantlygreater number of patients achieved remission from depression.
Dr Phyllis Zee: ere are some medications, includingeszopiclone and low-dose doxepin, that are indicated for sleepmaintenance insomnia, whereas other medications, such aszaleplon, are not (Table 9).
Dr Sonia Ancoli-Israel: I think that is a major point. Animportant aspect of selecting insomnia medications is matching
the medication with the patients sleep complaint. If a patient ishaving difficulty staying asleep, but not falling asleep, you have tthink about a medication in which the action is going to bemaintained during the second half of the night, as opposed to juthe rst half of the night.
Dr Tom Roth:When you look at the existing treatment options thwork on the sleep system, none of the GABAAreceptor agonistsreally have major sleep maintenance effects. ey actually have sleemaintenance effects for 3, 4, and 5 hours at the max. e reason forthat is very simple. If you have effects that last for 6, 7, and 8 hourswith medications that potentiate the GABA system, you are going have signicant next-day impairment. is, in part, explains why alot of clinicians tend to use off-label medications, including atypicaantipsychotics and antidepressants. Among approximately 900million office visits that took place in 2006, an estimated 30 millionvisits included a prescription for insomnia without depression liste
as comorbidity; nearly half of these prescriptions were forantidepressants. 32 Compared to medications that work on theGABA system, the majority of off-label medications have longer
An important aspect of selecting insomniamedications is matching the medication with thepatients sleep complaint. Dr Sonia Ancoli-Israel
-
8/12/2019 El Aerobic Mejora El Sueo 5
11/20
half-lives, resulting in sleep maintenance effects in 6, 7, and 8 hours.ese medications are effective because they target receptors
involved in the wake system, including histamine, dopamine, andserotonin. e wake systems are very important with regard to thepathophysiology of insomnia, and that may be why thesemedications are frequently prescribed in practice.
Dr Larry Culpepper: Since a number of clinicians prescribeoff-label medications for the treatment of insomnia, the role ofthe FDA in the United States should be mentioned. e FDA hasclearly stated that hypnotic medications should be started at thelowest possible dose and then titrated to the desired effect,provided the titration can be performed safely and the lower dosewas ineffective.
ese recommendations will become part of product labeling,and we have already seen this with the recent changes tozolpidem.33 For medications that are used off-label, thisinformation is not readily available because the medicationshavent been studied systematically.
Dr Tom Roth: e best example of this is low-dose doxepin. Inthe past, doxepin had been prescribed at doses as high as 25 mg to
100 mg for the treatment of insomnia. Aer a dose-responsestudy was performed, the hypnotic dose of doxepin wasdetermined to range from 3 mg to 6 mg.34 Its not whetherdoxepin is a good drug or a bad drug. e point is the drugseffects are dose dependent. At doses higher than 6 mg, doxepinhas signicant anticholinergic effects. At doses ranging from 3 mgto 6 mg, doxepin has limited anticholinergic effects and worksprimarily on the histamine receptor. So again, the problem withusing off-label medications is our lack of knowledge with regardto the dose-response relationships between safety and efficacy.I think doxepin provides us with a clear example of that.
Nonprescription MedicationsDr Larry Culpepper: Nonprescription therapies are frequentlyused by patients to treat insomnia-related symptoms, but there islimited safety and efficacy data to support these therapies. Forinstance, people occasionally use alcohol as a sleep aid, thinkingthis will improve their sleep. While alcohol has been reported tohelp people fall asleep more quickly, this effect is offset by havingmore disrupted sleep in the second half of the night.35
Dr Phyllis Zee:And then there is the issue of anticholinergic sideeffects, especially in the elderly, with many of the over-the-counter(OTC) sleep medications. Elderly patients may already havesome cognitive impairment and balance issues, and medicationswith anticholinergic side effects only worsen many of theircoexisting conditions.
e FDA has clearly stated that hypnoticmedications should be started at the lowest possible
dose and then titrated to the desired effect,provided the titration can be performed safely and
the lower dose was ineffective. Dr Larry Culpepper
Brand name Generic name Half-life FDA-approved indications Available doses
Histamine receptor antagonist (H1)
Silenor Doxepin 15 hrs Sleep maintenance 3 mg, 6 mg
Melatonin receptor agonist (M1 and M2)
Rozerem Ramelteon 2.6 hrs Sleep onset 8 mg
GABAA-receptor agonists: nonbenzodiazepines
*For all zolpidem products, the lowest available dose is recommended when initiating treatment in womenSonata Zaleplon 1 hr Sleep onset 5 mg, 10 mg
Edluar(Sublingual tablet)
Zolpidem 2.5 hrs Sleep onset 5 mg, 10 mg
Ambien Zolpidem 2.5 hrs Sleep onset 5 mg, 10 mg
ZolpiMist(Oral spray)
Zolpidem 2.5 hrs Sleep onset 1 spray = 5 mg
Intermezzo(Sublingual tablet)
Zolpidem 2.5 hrs Middle-of-the-night awakenings 1.75 mg, 3.5 mg
Ambien CR(Controlled-release)
Zolpidem 2.5 hrs Sleep onsetSleep maintenance
6.25 mg, 12.5 mg
Lunesta Eszopiclone 5-7 hrs Sleep onsetSleep maintenance 1 mg, 2 mg, 3 mg
GABAA-receptor agonists: benzodiazepines
Halcion Triazolam 2-4 hrs Sleep onset 0.125 mg, 0.25 mg
Restoril Temazepam 8-20 hrs Sleep onsetSleep maintenance
7.5 mg, 15 mg, 22.5 mg, 30 mg
Doral Quazepam 39-73 hrs Sleep onsetSleep maintenance
7.5 mg, 15 mg
Table 9. Commonly Prescribed FDA-Approved Insomnia Medications
-
8/12/2019 El Aerobic Mejora El Sueo 5
12/20
12 Dr Sonia Ancoli-Israel: ese side effects need to be avoided inthis population. Diphenhydramine, for example, has increasedrebound effects in the elderly (worsening of sleep compared topretreatment symptoms).36Yet, the elderly are some of thehighest users of OTC sleep medications.37
Dr Andrew Krystal:A signicant number of OTC sleepmedications contain either diphenhydramine or doxylamine,which have substantial anticholinergic effects. Consumers who
see OTC sleep medications in the drug store frequently assumethey are safer than prescription medications, but this is notnecessarily the case.
Dr Phyllis Zee: In addition to OTC antihistamines, there arenumerous other medications that patients use to self-medicate,rather than seeking medical aention. e 2002 National HealthInterview Survey data showed that more than 1.6 million US adultsuse complementary and alternative medicine for sleep-relatedsymptoms.38A total of 65% of those patients used biologicallybased therapies, including herbal remedies, which have limitedsafety and efficacy data and are not regulated by the FDA.
Dr Tom Roth: Falls and the risk for falling are important issueswith regard to insomnia and its treatments. e majority of dataseem to indicate that the causative factor, with regard tomedications, is total sedative load.39,40 If a patient is takingmedications with signicant anticholinergic side effects while alsotaking a sleep agent, there is a risk for falling. It is not linked to anysingle medication. Additionally, there are studies that showinsomnia is more of a risk factor than sleep agents.41 If you give amedication for insomnia to patients and they sleep for 8 hoursand do not get out of bed, they do not fall. However, if you havepatients who have to get up 3 or 4 times a night because of anunderlying medical condition, then sleep agents are a risk.
Differentiating Treatments for InsomniaFrom Treatments for CircadianRhythm DisordersCRSDs occur when the timing of the endogenous circadianrhythm and the normal 24-hour sleep-wake cycle are offset.Circadian rhythms are coordinated by the suprachiasmaticnucleus (SCN), which is reset by light through theretinohypothalamic tract.42Although less potent than light,melatonin, which is released by the pineal gland during the darkcycle, resets circadian rhythm as well.43 Because they play keyroles in stabilizing circadian rhythm, timed exposure to melatoninand light are effective treatment methods in patients with CRSDs.
Dr Tom Roth: I would like to take a minute and have Dr Zeebriey explain the roles of melatonin and light in CRSDs.
Dr Phyllis Zee: Light is the strongest entraining agent for thecircadian clock. Exposure to bright light in the early morninginduces phase advances, whereas light exposure in the eveningdelays the phase of circadian rhythms.44 In patients with CRSDs,the timing of light exposure (as a treatment intervention) istargeted toward the patients presenting symptoms. For example,elderly patients oen present with an advanced phase disorder,which means they go to bed early at night and wake up early in the
morning. In this circumstance, increasing light exposure in the
evening (to keep them up later) and limiting light exposure in thmorning (to entrain a later wake time) would be an initialintervention in this type of patient. In patients with a delayedphase disorder, the exact opposite would be prescribed. Withregard to melatonin, it has demonstrated clinical benet inpatients with CRSDs. Melatonin does not have a major role in thtreatment of insomnia disorder45; however, in a patient who onlyhas trouble falling asleep, one should consider the possibility of delayed circadian rhythm. If an underlying circadian
misalignment is present, a trial of low-dose melatonin may beuseful. A low dose of melatonin would be 0.3 mg to 1 mg. Its noapproved by the FDA for the treatment of insomnia disorder.
Dr Andrew Krystal: I think it s important to emphasize thatmelatonin should notbe taken right before going to bed.
Dr Phyllis Zee: I agree. Many patients with delayed sleep phasedisorder come to me indicating that theyve tried melatonin, butit didnt work. ey usually have taken it right before bedtime,which is too late to advance the phase of circadian rhythms. Toadvance the timing of the sleep-wake cycle, the ideal time to takmelatonin is 5 to 6 hours before the patients natural sleep time.
Dr Sonia Ancoli-Israel: To add to what Dr. Zee was mentioningmoment ago with regard to light, the best way for the advancedphase patients to avoid morning light is by wearing sunglasses
when they go outside because the mechanism is through the eyee light-dark cycle information is relayed from the retina to theSCN primarily by the retinohypothalamic tract.
Dr Tom Roth: Many elderly people are terried of falling duringthe night, so they keep a night light on. It is very important thatelderly people keep a night light by their bathroom but outside othe line of vision. We need light during the day, but we also needdarkness at night.
Dr Phyllis Zee: If the patient needs a night light, recommenda red lter because melatonin does not get suppressed veryeasily with long-wavelength light, such as red. In contrast,
short-wavelength light, such as blue, is more effective insuppressing the secretion of melatonin from the pineal gland.Short wavelength light also activates the sympathetic nervoussystem, resulting in increased arousal.46
Emerging erapies for InsomniaTwo separate research groups discovered orexin (also referred toas hypocretin) neuropeptides, which are wake-promotingneurotransmiers produced by a cluster of neurons in thehypothalamus.47,48 Orexin peptides inuence the patientssleep-wake cycle, appetite, and autonomic nervous system,including effects on metabolic rate and behavioral responses to
stress.47 e brain contains 50,000 to 80,000 orexin producing
I think its important to emphasize that melatoninshould not be taken right before going to bed.
Dr Andrew Krystal
-
8/12/2019 El Aerobic Mejora El Sueo 5
13/20
neurons, which have extensive projections to many different regionsin the brain. e strongest projections appear to target wake-promoting regions that regulate arousal, including noradrenergicneurons of the locus coeruleus, histaminergic neurons of thetuberomammilary nucleus, dopaminergic neurons of the ventraltegmental area, and serotonergic neurons of the raphe nuclei.49
e orexin neurons are predominantly active during periods ofwakefulness and become less active during NREM and REMsleep. Patients who have narcolepsy experience chronic sleepiness
and have an approximately 90% loss of functioning orexinneurons, further suggesting the wake-promoting role of orexinneuropeptides.50 Because orexin plays a signicant role in thewake cycle, recent research has exploited the clinical benets ofantagonizing this receptor.
In phase III clinical trials, suvorexant, a dual orexin receptorantagonist, signicantly improved sleep onset and sleepmaintenance compared to placebo.51,52 However, while theefficacy of suvorexant was established, next-day impairmentwas a concern, warranting further evaluation of select doses. Inaddition, research has shown that antagonizing serotonin
receptors (5HT-7) signicantly improves sleep maintenance,suggesting a potential role for agents with this effect in thetreatment of insomnia.53 In this nal section, the roundtablepanelists discuss emerging therapies and their potential roles inthe management of insomnia.
Dr Larry Culpepper: Turning the discussion toward emergingtreatments, how do the orexin receptor antagonists and serotoninreceptor antagonists affect the sleep-wake system?
Dr Tom Roth: For the past 30 years, weve had medications thatwork primarily on the sleep system through GABA mechanisms.However, with the emergence of low-dose doxepin, orexin
receptor antagonists, and serotonin receptor antagonists, there aremore medications focused on reducing arousal associated withthe wake system, rather than simply pushing sleep harder. Orexinreceptor antagonists are probably the medications that are closestto the nish line, and orexin is a major transmier system that isinvolved in the arousal system. It feeds into the noradrenergic,histaminergic, and serotonergic systems.
Dr Phyllis Zee: In addition, when orexin neurons are ring duringwakefulness, they inhibit the VLPO, which is the sleep-promotingcenter in the brain. Its not only activating the wake promotingregions in the brain, but its also inhibiting the sleep center.6
erefore, if you antagonize the orexin system, you can promote
sleep by affecting both sleep and wake.
Dr Tom Roth:When you give a patient zolpidem, you want it to goto the VLPO, but it binds receptors in the cerebellum as well, whichcauses ataxia. It does these things because the GABA system is sowidespread. In contrast, orexin is produced by a small group of cellsthat are located in the lateral hypothalamus, with signicantprojections to regions of the brain that promote arousal.49Whenthese medications are administered, they cause regional effects onthe brain versus the widespread effects we typically see withmedications that potentiate the GABA system, which has a lot to dowith receptor density.
Dr Larry Culpepper:We will need to adjust our thinking withregard to these newer agents because they re drastically different,at least from a pharmacokinetic perspective. For example,suvorexant, an orexin receptor antagonist, has a half-life of12 hours.52 If this was a benzodiazepine that was affecting theGABA system, the sleep side of the switch, you could not usethese medications because of the signicant next-day impairment.
Dr Tom Roth: If you look at low-dose doxepin, it has profoundeffects on sleep at the end of the night. If you look at the orexinand serotonin receptor antagonists, they have profound effects onsleep at the end of the night. at is a very important timebecause in those later hours you have already slept for 4 or5 hours, and your homeostatic drive (the increased need for sleepdue to extended periods of wakefulness) is way down. Mostpeople experience wake time in the last 3 hours of the night, andthese medications are targeting those nal hours of sleep. eother factor you have to remember is benzodiazepine receptoragonists work by simply shuing the brain down, and that makesyou fall asleep very, very quickly, which is what Dr Culpepper wasalluding to earlier. When transitioning patients frombenzodiazepine receptor agonists to these newer medications,patient education will become very important because thepharmacokinetic/pharmacodynamic indices of these medicationsare profoundly different. e onset of action of these newer
compounds is not as fast as the medications that work on theGABA system; conversely, the duration of action of these neweragents appears to be longer.
Dr Sonia Ancoli-Israel: ese medications may not help patientsget to sleep as fast as medications affecting the GABA systembecause orexin receptor antagonists, for example, are morefocused on extending sleep. Education will be necessary to reducethe patients expectation of rapidly falling asleep.
Final oughtsResearch suggests that insomnia is a condition of hyperarousalcaused by a relative shi in the balance of activity of thesleep-promoting and wake-promoting systems towards an increasein activity in wake-promoting systems. Insomnia is not a symptomof other disorders, but it s comorbid with other medical conditions,requiring its own intervention. Several studies, which haveevaluated behavioral and pharmacologic therapy, support thisdirection in treatment. In addition, clinicians will not only need toinquire about insomnia when comorbid conditions are present butthey will also need to inquire about comorbid conditions wheninsomnia is present.
We will need to adjust our thinking with regardto these newer agents because theyre drastically
different, at least om a pharmacokineticperspective. Dr Larry Culpepper
-
8/12/2019 El Aerobic Mejora El Sueo 5
14/20
14
1. Manifestation and management of chronic insomnia in adults.Agency for Healthcare Quality and Research Web site.hp://archive.ahrq.gov/clinic/epcsums/ insomnsum.htm#ref2.Updated June 2005. Accessed July 15, 2013.
2. Kessler RC, Berglund P, Demler O, et al. e epidemiology ofmajor depressive disorder: results from the National ComorbiditySurvey Replication (NCS-R).JAMA. 2003;289:3095-3105.
3. Kessler RC, Berglund PA, Coulouvarat C, et al. Insomnia and theperformance of US workers: results from the America InsomniaSurvey. Sleep. 2011;34(9):1161-1171.
4.American Psychiatric Association. Diagnostic and Statistical Manualof Mental Disorders. Fih Edition.American Psychiatric
Association Web site. hp://www.psychiatry.org/practice/dsm/dsm5. Accessed July 7, 2013.
5. Rogers L, Holmes M. Model of the human sleep wake system.arXiv:1208.3228v1 [math.DS]. August 15, 2012.
6. Saper CB, Scammell TS, Lu J. Hypothalamic regulation of sleepand circadian rhythms.Nature. 2005;437:1257-1263.
7. Bonnet MH, Arand DL. Heart rate variability in insomniacs andmatched normal sleepers.Psychosom Med. 1998;60:610-615.
8. Bonnet MH, Arand DL. Physiological activation in patients withsleep state misperception.Psychosom Med. 1997;59(5):533-540.
9. Vgontzas AN, Bixler EO, Lin HM, et al. Chronic insomnia isassociated with nyctochemeral activation of the hypothalamic-pituitary-adrenal axis: clinical implications.J Clin Endocrinol
Metab. 2001;86:3787-3794.
10. Nofzinger EA, Buysse DJ, Germain A, Price JC, Miewald JM,Kupfer DJ. Functional neuroimaging evidence for hyperarousal ininsomnia.Am J Psychiatry. 2004;161:2126-2128.
11. Stepanski E, Zorick F, Roehrs T, Young D, Roth T. Daytimealertness in patients with chronic insomnia compared withasymptomatic control subjects. Sleep. 1988;11(1):54-60.
12. e National Sleep Foundations 2005 Sleep in America Poll.National Sleep Foundation Web site. hp://www.sleepfoundation.org/sites/default/les/2005_summary_of_ndings.pdf. Accessed July 15, 2013.
13. Morin CM, Bellevi lle G, Blange L, Ivers H. Insomnia severityindex: psychometric indicators to detect insomnia cases andevaluate treatment response. Sleep. 2011;34(5):601-608.
14. Hajak G, Petukhova M, Lakoma M, et al. Days out-of-role
associated with insomnia and comorbid conditions in theAmerican Insomnia Survey.Biol Psychiatry. 2011;70:1063-1073.
15. Nierenberg AA, Husain MM, Wisniewski SR, et al. Residualsymptoms aer remission of major depressive disorder withcitalopram and risk of relapse: a STAR*D report.Psychol Med.2010;40:41-50.
16. Chang PP, Ford DE, Mead LA, Cooper-Patrick L, Klag MJ.Insomnia in young men and subsequent depression. e JohnsHopkins Precursor Study.Am J Epidemiol. 1997;146:105-114.
17. Knutson KL, Van Cauter E, Zee P, Liu K , Lauderdale DS. Cross-sectional associations between measures of sleep and markers ofglucose metabolism among subjects with and without diabetes:the coronary artery risk development in young adults sleep stud(CARDIA).Diabetes Care. 2011;34:1171-1176.
18. Vgontzas A, Liao D, Pejovic S, Calhoun S, Karataraki M, BixlerEO. Insomnia with objective short sleep duration is associated
with type 2 diabetes: a population study.Diabetes Care. 2009;32:1980-1985.
19. Jackson CW, Curtis JL. Sleep disorders. In: Dipiro JT, TalbertRL, Yee GC, Matzke GR, Wells BG, Posey LM, eds.
Pharmacotherapy: A Pathophysiologic Approach. 6th ed.New York, NY: McGraw-Hill; 2005.
20. Sack R, Auckley D, Auger RR, et al. Circadian rhythm sleepdisorders: Part II, advanced sleep phase disorder, delayed sleepphase disorder, free-running disorder, and irregular sleep-wakerhythm. Sleep. 2007;30(11):1484-1501.
21. Schue-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinic
guideline for the evaluation and management of chronic insomnin adults.J Clin Sleep Med. 2008;4(5):487-504.
22. Morin C, Bootzin R , Buysse D, Edinger J, Espie C, Lichstein K.Psychological and behavioral treatment of insomnia: update ofthe recent evidence (1998-2004). Sleep. 2006;29:1398-1414.
23. Spielman AJ, Saskin P, orpy MJ. Treatment of chronic insomnby restriction of time in bed. Sleep. 1987;10(1):45-56.
24. Buysse DJ, Germain A, Moul DE, et al. Efficacy of brief behaviotreatment for chronic insomnia in older adults.Arch Intern Med.2011;171(10):887-895.
25. Manber R , Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TKalista T. Cognitive behavioral therapy for insomnia enhances
depression outcome in patients with comorbid major depressivedisorder and insomnia. Sleep. 2008;31(4):489-495.
26. Reid KJ, Glazer-Baron J, Lu B, Naylor E, Wolfe S, Zee P. Aerobicexercise improves self-reported sleep and quality of life in olderadults with insomnia. Sleep Med. 2010;11(9):934-940.
27. Bormann J. e ABC of GABA receptors. Trends Pharmacol Sci2000;21:16-19.
28. Nu D. GABA-A receptors: subtypes, regional distribution, andfunction.J Clin Sleep Med. 2006;2(2)(suppl):S7-S11.
29. Fava M, Asnis GM, Shrivastava R, et al. Zolpidem extended-release improves sleep and next-day symptoms in comorbid
insomnia and generalized anxiety disorder.J ClinPsychopharmacol. 2009;29:222-230.
30. Pollack M, Kinrys G, Krystal A, et al. Eszopiclone coadministerewith escitalopram in patients with insomnia and comorbidgeneralized anxiety disorder.Arch Gen Psychiatry. 2008;65:551-562.
31. Fava M, McCall WV, Krystal A, et al. Eszopiclone coadministerewith uoxetine in patients with insomnia coexisting with majordepressive disorder.Biol Psychiatry. 2006;59:1052-1060.
References
-
8/12/2019 El Aerobic Mejora El Sueo 5
15/20
32. Lai LL, Tan MH, Lai YC. Prevalence and factors associated withoff-label antidepressant prescriptions for insomnia.Drug Health
Patient Safety. 2011; 3:27-36.
33. FDA Drug Safety Communication: FDA approves labelchanges for zolpidem products, including new dosingand a recommendation to avoid driving the day aer
Ambien CR use. US Food and Drug AdministrationWeb site. hp://www.fda.gov/. Updated May 17, 2013.Accessed May 19, 2013.
34. Silenor [package insert]. San Diego, CA: SomaxonPharmaceuticals, Inc; 2010.
35. Meoli AL, Rosen C, Kristo D, et al. Oral nonprescriptiontreatment for insomnia: an evaluation of products with limitedevidence.J Clin Sleep Med. 2005;1(2):173-187.
36. Glass JR, Sproule BA, Herrmann N, et al. Effects of two weektreatment with temazepam and diphenhydramine in elderlyinsomniacs: a randomized, placebo-controlled trial.J Clin
Psychopharmacol. 2008;28(2):182-188.
37. Ancoli-Israel S. Insomnia in the elderly: a review for the primarycare practitioner. Sleep. 2000;23(suppl 1):S23-S30.
38. Pearson NJ, Johnson LL, Nahin RL. Insomnia, trouble sleeping,and complementary and alternative medicine: analysis of the2002 National Health Interview Survey data.Arch Intern Med.2006;166:1775-1782.
39. Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. eanticholinergic risk scale and anticholinergic adverse effects inolder persons.Arch Intern Med. 2008;168(5):508-513.
40. Corsinovi L, Bo M, Aimonino NR, et al. Predictors of falls andhospitalization outcomes in elderly patients admied to an acutegeriatric unit.Arch Gerontol Geriatr. 2008. doi:10.1016/
j.archger.2008.06.004.41. Avidan AY, Fries BE, James ML, Szafara KL, Wright GT, Chervin
RD. Insomnia and hypnotic use, recorded in the minimum dataset, as predictors for falls and hip fractures in Michigan nursinghomes.J Am Geriatr Soc. 2005;53(6):955-962.
42. Sadun AA, Schaechter JD, Smith LE. A retinohypothalamicpathway in man: light mediation of circadian rhythms.Brain Res.1984;302:371-377.
43. Lewy AJ, Wehr TA, Goodwin FK, et al. Light suppressesmelatonin secretion in humans. Science. 1980;210:1267-1269.
44. Czeisler CA, Richardson GS, Coleman RM, et al. Chronotherapy:
reseing the circadian clocks of patients with delayed sleep phase
insomnia. Sleep. 1981;4(1):1-21.
45. Ferraciolo-Oda E, Qawasmi A, Bloch MH. Meta-analysis:
melatonin in the treatment of primary sleep disorders.PLoS One.
2013;8(5):e63773. doi:10.1371/journal.pone.0063773.
46. Cajochen C, Munch M, Kobialka, et al. High sensitivity of humanmelatonin, alertness, thermoregulation, and heart rate to short
wavelength light.J Clin Endocrinol Metab. 2005;90(3):1311-1316.
47. Sakurai T, Amemiya A, Ishii M, et al. Orexins and orexin
receptors: a family of hypothalamic neuorpeptides and
G protein-coupled receptors that regulate feeding behavior.
Cell. 1998;92:573-585.
48. de Lecea L, Kilduff TS, Peyron C, et al. e hypocretins:
hypothalamus-specic peptides with neuroexcitatory activity.
Proc Natl Acad Sci USA. 1998;95:322-327.
49. Peyron C, Tighe DK, van den Pol, et al. Neurons containing
hypocretin (orexin) project to multiple neuronal systems.J Neurosci. 1998:18:9996-10015.
50. annickal TC, Moore RY, Nienhuis R, et al. Reduced number of
hyocretin neurons in human narcolepsy.Neuron. 2000;27:
469-474.
51. Herring JW, Snyder E, Budd K, et al. Orexin receptor antagonism
for treatment of insomnia: a randomized clinical trial of
suvorexant.Neurology. 2012;79(1):1-10.
52. US Food and Drug Administration Web Site. Suvorexant
Advisory Commiee meeting brieng document: Peripheral &
Central Nervous System Drugs Advisory Commiee meeting,
May 22, 2013. hp://www.fda.gov/downloads/ AdvisoryCommiees/CommieesMeetingMaterials/Drugs/
PeripheralandCentralNervousSystemDrugsAdvisoryCommiee/
UCM352970.pdf. Accessed May 20, 2013.
53. Krystal AD, Zammit G, Pikalov A . e effects of 5HT-7
antagonism on sleep in humans: a placebo-controlled cross-over
study of lurasidone in a 4-hour phase-advance model of healthy
volunteers. Program and abstracts of the 27th Annual Meeting of
the Associated Professional Sleep Societies, LLC; June 1-5, 2013;
Baltimore, MD. Abstract 0556.
To Obtain CME CreditPIM supports Green CME by offering your Request for
Credit online. If you wish to receive acknowledgment for
completing this activity, please complete the post-test and
evaluation on www.cmeuniversity.com . On the navigation
menu, click on Find Post-test/Evaluation by Course and
search by course ID 9496.
http://www.cmeuniversity.com/searchResult.aspx?t=1&f=eval&s=9496http://www.cmeuniversity.com/searchResult.aspx?t=1&f=eval&s=9496http://www.cmeuniversity.com/searchResult.aspx?t=1&f=eval&s=9496http://www.cmeuniversity.com/searchResult.aspx?t=1&f=eval&s=9496http://www.cmeuniversity.com/searchResult.aspx?t=1&f=eval&s=9496http://www.cmeuniversity.com/searchResult.aspx?t=1&f=eval&s=9496http://www.cmeuniversity.com/searchResult.aspx?t=1&f=eval&s=9496http://www.cmeuniversity.com/searchResult.aspx?t=1&f=eval&s=9496http://www.cmeuniversity.com/searchResult.aspx?t=1&f=eval&s=9496http://www.cmeuniversity.com/searchResult.aspx?t=1&f=eval&s=9496http://www.cmeuniversity.com/searchResult.aspx?t=1&f=eval&s=9496http://www.cmeuniversity.com/searchResult.aspx?t=1&f=eval&s=9496 -
8/12/2019 El Aerobic Mejora El Sueo 5
16/20
New Directions
Management ofin the
BalancingPathophysiologyTerapeuticsand
Insomnia
-
8/12/2019 El Aerobic Mejora El Sueo 5
17/20
!"# %&'"()&*+, &+ )-" ./+/0"1"+) *2 3+,*1+&/!"#"$%&$' )"*+,-+./&,#,'. "$0 1+23"-24*&%/
!"#$%%&'()* ,"#- .( /01%"2 3#4(&2.56% 7'*$4**'#(
4.5 6",)
6* 78)/&+ 4.5 4'"9&):
)56 /4--,3*/ 7322$ 869 :. ,;;23&$' .,43 5; .,4 ?&/+ *, 32%2&@2
"%A$,?#20'2B2$* ;,3 %,B-#2*&$' *+&/ "%*&@&*.C -#2"/2 %,B-#2*2 *+2 -,/*D*2/* "$0 2@"#4"*&,$ ,$
+**-EFF???>%B24$&@23/&*.>%,BF/2"3%+"/-GH*IJK;I2@"#K/ILMLN>
O$ *+2 $"@&'"*&,$ B2$4C %#&%A ,$ PQ&$0 ),/*D*2/*F9@"#4"*&,$ :. 8,43/2R "$0 /2"3%+ :. %,43/2 5S LMLN>
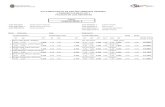
;? / @ABC"/'B*D9 2"1/D"? (&'(D", )-" +E18"' FGH 2*' "/(- IE",)&*+ *+ )-" 3+,*1+&/ J"K"'&)C
3+9"L< =>M, )*)/D ,(*'" &+9&(/)", #-&(- D"K"D *2 &+,*1+&/N
/%,BF/2"3%+"/-GH*IJK;I2@"#K/ILMLN>
O$ *+2 $"@&'"*&,$ B2$4C %#&%A ,$ PQ&$0 ),/*D*2/*F9@"#4"*&,$ :. 8,43/2R "$0 /2"3%+ :. %,43/2 5S LMLN>
Take CME T