Circulacion Cerebral
Click here to load reader
-
Upload
martha-elena -
Category
Documents
-
view
218 -
download
2
Transcript of Circulacion Cerebral

Invited Review
HIGHLIGHTED TOPIC Regulation of the Cerebral Circulation
Chronic hypoxia and the cerebral circulation
Kui Xu and Joseph C. LaMannaDepartment of Anatomy, Case Western Reserve University School of Medicine, Cleveland, Ohio
Xu, Kui, and Joseph C. LaManna. Chronic hypoxia and the cerebral circula-tion. J Appl Physiol 100: 725–730, 2006; doi:10.1152/japplphysiol.00940.2005.—Exposure to mild hypoxia elicits a characteristic cerebrovascular response inmammals, including humans. Initially, cerebral blood flow (CBF) increases asmuch as twofold. The blood flow increase is blunted somewhat by a decreasingarterial PCO2 as a result of the hypoxia-induced hyperventilatory response. After afew days, CBF begins to fall back toward baseline levels as the blood oxygen-carrying capacity is increasing due to increasing hemoglobin concentration andpacked red cell volume as a result of erythropoietin upregulation. By the end of 2wk of hypoxic exposure, brain capillary density has increased with resultantdecreased intercapillary distances. The relative time courses of these changessuggest that they are adjusted by different control signals and mechanisms. TheCBF response appears linked to the blood oxygen-carrying capacity, whereas thehypoxia-induced brain angiogenesis appears to be in response to tissue hypoxia.
altitude adaptation; angiogenesis; cerebral blood flow; cerebral blood volume
HISTORICAL PERSPECTIVE
THE RELATIONSHIP BETWEEN brain function and blood flow hasbeen studied since the classical paper of Roy and Sherrington(61) at the end of the 19th century. Despite the absence ofquantitative methods, early investigators were able to establishsome of the basic principles of the cerebral circulation; amongthese was a recognition of the dominating influence of carbondioxide and the reciprocal effect of oxygen (72). Interestingly,even the idea that local cerebral blood flow (CBF) was tran-siently augmented with increased neuronal activation, alludedto by Roy and Sherrington, had received additional qualitativeexperimental support. A listing of the qualitative methods inuse at the time, including methods such as venous outflow,radium emanation, and thermocouple, can be found in the 1936Wolff review (72).
Nevertheless, despite more than 100 years of effort, there arestill major areas concerning the control of the cerebral circu-lation that remain unknown. The observations that decreasingoxygen led to increased blood flow and that the increase wasblunted perhaps by the accompanying hypoxia-induced hyper-ventilation and resultant decreased carbon dioxide remainedwholly qualitative until a useful quantitative method, based oninert gases, was developed for measuring CBF and oxygenmetabolism by Kety and Schmidt (33, 35). They recorded theblood flow increase in seven young men from the resting levelof 54 � 4 ml �100 g�1 �min�1 (mean � SE) to 73 � 5 ml �100g�1 �min�1 while breathing 10% oxygen, with an averageincrease of 137 � 9% (34). These investigators chose to reportthe blood flow measurements per 100 g tissue presumably toprovide convenient units with whole numbers rather than
decimals (35). This tradition has been followed ever since,although many investigators are beginning to switch to themore scientific international friendly units (ml �g�1 �min�1).
Severinghaus and his colleagues (64) used the Kety andSchmidt method to measure CBF in seven volunteers breathingatmospheric air at sea level and at the Barcroft Laboratory atWhite Mountain, California, which is at an altitude of 3,810 m.This was the first quantitative study of the time course of thehypoxic CBF response. They reported a mean sea-level CBF of42 � 2 ml �100 g�1 �min�1, increasing to 51 � 4 ml �100g�1 �min�1 after 6–12 h at altitude, and falling back toward thesea-level CBF after 3–5 days acclimation (47 � 3 ml �100g�1 �min�1). They realized that as the PCO2 had fallen to 30Torr, the return of CBF implied a “resetting” of the centralmedullary chemoreceptor. The data from this study have beenanalyzed in great detail recently (70, 71).
Current models of chronic hypoxia. This review concernsitself with the cerebrovascular adaptations that occur in re-sponse to chronic hypoxia. The term “hypoxia” is used to covera wide variety of situations, and usually it needs to be definedthrough the use of specific delimiters. In general, hypoxiasimply describes a lower than normal oxygen pressure. For thispaper, we will consider hypoxia to refer to lower than normalatmospheric oxygen. This condition might be produced bydecreasing the fractional component of oxygen in the inspiredgas mixture, producing “hypoxic hypoxia.” Several systemsare currently available to control the composition of gases innormobaric chambers, allowing the study of intermittent hy-poxic exposures on an infinite variety of duty cycles. Hypoxiacan also be produced by decreasing the overall barometricpressure, resulting in “hypobaric hypoxia.” Hypobaric hypoxiacan be produced either naturally by ascent to altitude or in“Wright chambers,” which are chambers for housing smallanimals fitted for withstanding a partial vacuum (73). Most of
Address for reprint requests and other correspondence: J. C. LaManna, Dept.of Anatomy, School of Medicine, Case Western Reserve Univ., 10900 EuclidAve., Cleveland, OH 44106-4930 (e-mail: [email protected]).
J Appl Physiol 100: 725–730, 2006;doi:10.1152/japplphysiol.00940.2005.
8750-7587/06 $8.00 Copyright © 2006 the American Physiological Societyhttp://www. jap.org 725

the literature studies on hypoxic adaptation have been con-ducted at altitude, in research stations around the world or inlaboratory simulations of climbs (for an exceptional review,see Ref. 69). There do not appear to be important differencesin the physiological adaptive response to the various methodsof producing continuous hypoxic exposure.
The degree of hypoxia also has had many descriptors,however, most investigators refer to three degrees (mild, mod-erate, and severe), without complete agreement on where theboundaries are drawn for each level. For the most part, hypoxiais considered mild if the arterial oxygen tension (PaO2
) does notfall below �50 Torr (assuming sufficient red cell volume).This degree is considered mild because there is almost com-plete compensation and function is relatively undisturbed. Theequivalent of 10% normobaric oxygen, or an altitude of�5,000 m, is the upper limit for mild hypoxia. Moderatehypoxia, PaO2
between �35 and 50 Torr, will manifest as adeterioration of thought processes, and below �35 Torr un-consciousness results. Although the results are not completelyclear, mild hypoxia is not associated with permanent neuronaldamage, but moderate and severe degrees of hypoxia lead toneuronal loss in a time of exposure/degree of hypoxia-depen-dent manner.
The term “chronic” is used loosely here to indicate aninterval of time for a physiological response to occur. In thecase of hypoxia, acute exposure occurs during an interval froma few minutes up to hours or even days, where chronicexposure occurs over weeks to months. Longer term adaptationoccurs over generations and can be observed and studied inanimal (e.g., Ref. 62) and human (e.g., Ref. 1), populations inthe Himalayas, Andes, and Ethiopia.
This short review will concentrate on the physiologicaladaptations of the cerebral circulation to prolonged exposure tomild hypoxic environments. It will rely mainly on data fromthe rodent model because most of the quantitative animalstudies have been done with the rat, but it will include sectionson species comparisons and human studies.
CEREBROVASCULAR ADAPTATION TO CHRONIC HYPOXIA
If it is considered that decreased oxygen delivery is theenvironmental stimulus for triggering the adaptive responses,then it remains to be determined what are the significantvariables contributing to the control mechanisms. These arewell known from basic physiology. From the point of view ofthe systemic circulation, the first variable, obviously, is thePaO2
, which is the partial pressure of oxygen as a gas dissolvedin the arterial blood. Second is the concentration of the oxygen-carrier hemoglobin, which is located in the red blood cells andis given as milligrams per deciliter or as the packed red cellfraction, often referred to as the hematocrit. The saturationcurve for hemoglobin is a third factor, and this curve is alteredby temperature, pH, arterial PCO2 (PaCO2
), and circulating2,3-diphospho-D-glycerate. Within the central nervous system,the important considerations are the blood flow rate and thecapillary density (hence intercapillary distance).
CBF. As noted above, CBF increases with exposure tohypoxia (15). Mild hypoxia results in an increase in CBF up tobut not quite double despite a fall in PaCO2
(2, 5, 10, 36). Theexact mechanism responsible for the increased CBF is un-
known; however, it appears to have a major neurogenic com-ponent originating in the brain stem (54).
Local signals will also have an influence [e.g., more of thevasodilator nitric oxide (NO) will be present as the amount ofoxygenated hemoglobin decreases], but environmental hypoxiais a systemic challenge and many mechanisms contribute to theadaptation. Local tissue factors may have more to do withintracerebral circulatory distribution rather than whole organblood flow. Although local chemical and metabolic factorssuch as K�, adenosine, and NO, among other things, certainlybecome increasingly important with severity of hypoxia (58),the mechanism for at least half of the acute increase in brainflow in response to mild hypoxia is most likely via neuronalpathways that originate or pass through the brain stem (18, 19,68) and closely related to the blood oxygen content (6, 28, 31).It may be part of a more generalized stress response (7).Hypoxia-induced hyperventilation reduces PaCO2
(53), whichopposes cerebral vasodilation, thus limiting the increase inblood flow.
When hypoxic exposure is prolonged for more than a day orso, the CBF increase becomes attenuated (40, 74) so that by 3wk of exposure the CBF has returned to prehypoxia baseline.
Packed red cell volume. One possible reason for the renor-malization of CBF is the well-known observation that thepacked red cell volume increases with exposure to hypoxia(42). This means that the oxygen content of the circulatingblood has been restored by balancing the loss of oxygen withincreased carrier, so that the oxygen delivery in (ml O2 �100g�1 �min�1) can be restored at the prehypoxic blood flow rate.In the rat, the packed red cell volume increases from thenormoxic �45% to �70% (22–24, 40, 74). In fact, oxygendelivery remains within the normal range during the entirehypoxic exposure (74).
Angiogenesis and cerebral blood volume. Although theoxygen delivery to the brain is relatively compensated duringchronic hypoxic exposure, it could be presumed that thedelivery of oxygen to the mitochondria within the parenchymawill be diminished because the driving force for diffusion fromcapillary to tissue is the PO2 difference between capillary andtissue. Because the tissue PO2 is close to zero, the driving forceis essentially the PaO2
, which remains low during continuedhypoxic exposure. (There is a small, but significant, increase inPaO2
with chronic hypoxia to the extent of the hyperventilatorydrop in PaCO2
.) This decrease in the driving force may underliethe finding that there is an increase in capillary density throughangiogenesis that is completed by 3 wk of hypoxic exposure (4,11, 20, 40, 51, 56, 57, 60).
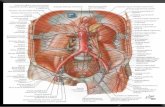
Angiogenesis occurs through the same hypoxia-induciblefactor-1 (HIF-1) transcription factor mechanism that leads toupregulation of erythropoietin and increased packed red cellvolume, but it works through upregulation of vascular endo-thelial growth factor. There is also a HIF-1-independent, cy-clooxygenase-2/angiopoietin-2 dependent component of cere-bral angiogenesis (59). Hypoxia-induced cerebral angiogenesishas been recently reviewed (39). The cartoon in Fig. 1 sum-marizes the key components of hypoxia-induced angiogenesis.
The increased capillary density should be detectable as anincrease in cerebral blood volume (CBV). Acute hypoxicexposure has been shown to result in an increase in CBV (32,65). The acute exposure result is most likely due to vasodila-tion. The effect of prolonged hypoxic exposure on CBV has
Invited Review
726 CHRONIC HYPOXIA AND THE CEREBRAL CIRCULATION
J Appl Physiol • VOL 100 • FEBRUARY 2006 • www.jap.org

also recently been reported (14) and related directly to capillarydensity.
Tissue oxygen tension. Even under normoxic conditions, themean tissue oxygen tension is low and the distribution isheterogeneous, with a left-shifted histogram (46, 66). Even so,regardless of the starting level, acute hypoxia results in adecrease of tissue oxygen (38, 43, 49, 66).
Assuming the hypoxic adaptations are successful, the endresult should be a restoration of tissue oxygen tension (41).This indeed appears to be the case. After 3 wk of hypoxia,tissue oxygen tension as measured by an in vivo electronparamagnetic resonance technique show levels equivalent tothe prehypoxic baseline (13). An important question for un-derstanding the control mechanism, not yet answered, is atwhat time interval during the adaptation phase the oxygentension is restored.
The relative time courses of the responses of CBF, packedred cell volume, capillary density, and HIF-1 are shown in Fig.2. CBF initially responds rapidly then falls off by the fourth orfifth day (74). Packed red cell volume has begun to increase byday 3, reaching �80% of maximum by 7 days (74). Angio-poietin-2 is upregulated for the 2 wk during which angiogen-esis is occurring, and then it falls to baseline by 3 wk (60).HIF-1, indicative of tissue hypoxia, is initially elevated, fallingto about half after 4 days and then back to baseline by 3 wk (8).These data imply that the restoration of brain tissue oxygen
tension does not occur until after 2 wk and before 3 wk ofhypoxic exposure. This interpretation implies that CBF is not afunction of tissue oxygen tension to any great extent but thatthe process of angiogenesis does directly respond to tissuesignals.
Mean transit time. Even though CBF has returned to prehy-poxic baseline levels, it does not mean that the cerebralcirculation has not undergone significant changes. Blood flowand blood volume are related to each other by consideration ofthe mean transit time through the Stewart-Hamilton principle(48). Thus, in its simplest form, the mean transit time can becalculated by dividing the blood volume by the blood flow.This variable refers to the average time it takes any unit ofblood to traverse from the arterial end of the capillary bed tothe venous end. For the rat, the average mean transit time is�1.5 s (3 ml/100 g divided by 130 ml �100 g�1 �min�1 times 60s/min). If CBV doubles after hypoxic adaptation, the meantransit time will become much longer, also doubling to �3 s.This means that there is much more unloading time for oxygenand, probably as significantly, for glucose. The effect onglucose delivery of the increased transit can be recognized inthe large increase in glucose influx across the blood-to-brainbarrier after adaptation to chronic hypoxia (22). Not only isthere an increase in the capillary density, but also there is anincrease in the number of GLUT1 transporter molecules permilligram of microvessel. Together with the increased resi-dence time in the capillary, the glucose influx increases bythree times compared with normoxic controls, reaching anextraction fraction of 0.7 or more.
SPECIES DIFFERENCES
Up to now, we have concentrated mostly on rat studies.Nevertheless, there are many commonalities with studies ofother species. The general mammalian pattern holds for themost, although there are some interesting differences. Withrespect to CBF, hypoxia induces an acute increase. This in-cludes sheep (29, 31, 37, 75) and cows (47). Hypoxic-adaptedanimals have a blood flow not too different from the normoxic.There are data in conflict with this, for example (37), whereCBF remains elevated for 4 days in sheep. It appears that the
Fig. 2. Relative time courses of cerebral blood flow, packed red cell volume[hematocrit (Hct)], HIF-1� (Hif), capillary density, and angiopoietin-2 (Ang 2)in response to chronic mild hypoxic exposure. Data from sources cited in text.
Fig. 1. Diagram depicts the components of hypoxia-induced angiogenesis. Inthe normoxic state, angiopoietin-1 (Ang-1) acting through the Tie-2 receptoron cerebral endothelial cells maintains structural integrity. During hypoxia,cyclooxygenase-2 (COX-2) is activated and arachidonic acid (AA) is con-verted to prostaglandin E2 (PGE2). PGE2 induces release of angiopoietin-2(Ang-2) from endothelial cells, which occupies the Tie-2 receptor resulting instructural instability and falling away of the pericyte. This allows access ofhypoxia-inducible factor-1 (HIF-1) upregulated VEGF to its receptors, stim-ulating the hypertrophy and hyperplasia of capillary angiogenesis.
Invited Review
727CHRONIC HYPOXIA AND THE CEREBRAL CIRCULATION
J Appl Physiol • VOL 100 • FEBRUARY 2006 • www.jap.org

discrepancy is related to the fact that these sheep develop acutemountain sickness (AMS). In sheep that did not develop AMS,the CBF tended to fall during the 4 days to about one-half ofthe hypoxic maximum, a result not too different from the rat.This is not to suggest that the increased CBF is a causativefactor in AMS because this is unlikely (30).
Other species differences occur due to various niche issuesthat are beyond the scope of this review but include species thatnormally reside at higher altitudes, such as the llama (44),those that are diving mammals such as the seal (25), and thosethat hibernate such as the ground squirrel (12). In addition tothese mammalian variations, there are an even greater numberwhen vertebrates are considered such as birds (3, 16), theturtle, and other anoxia-tolerant vertebrates (27, 55). Majordifferences also exist in comparison between the fetus and theadult (17, 45).
Scaling. To compare species properly, it is important todistinguish the differences that are due to size. For this we usethe principles of allometry to understand the pertinent scalingvariables (63). In general, blood flow and metabolic rate areproportional. Thus it is no surprise that blood flow is a scaledvariable. CBF, expressed per unit weight, scales with about the�0.25 power of body weight; the smaller the mammal, thehigher the blood flow. CBV and packed red cell volume do notscale, but they remain constant across mammals. Thus the ratioof these variables, the mean transit time, must also scale, andlarger brains will have longer transit times. The longer transittimes in the larger brains might be the reason for the unex-plained observation that the human red blood cell has asignificant amount of the GLUT1 transporter, whereas smallmammals like the rat and mouse do not have GLUT-1 trans-porters on their red blood cells (21).
Human studies. There is a long and rich literature concern-ing cerebrovascular physiology and adaptation to altitude (42,69). In general, the findings appear to echo the same mamma-lian pattern that has been discussed. In many ways the humanexperiments have preceded and surpassed those of the animalstudies. There are far more quantitative studies of CBF, cere-bral metabolic rate of oxygen (CMRO2), and cerebral meta-bolic rate of glucose in humans than in animals. The basicobservation of a hypoxia-induced, acute increase in CBF fol-lowed by adaptation to prehypoxic levels have been confirmedmany times (9, 50, 52, 67). Resting CBF measured in popula-tions living at altitude (highlanders) is quite similar to that ofthe average lowlander. In a recent study of nine healthy adultsin whom CBF was measured after 3 wk at Chalcaltaya inBolivia (5,260 m) and then some 8 mo or so after return to sealevel, CBF was found to be unchanged at 53 ml �100g�1 �min�1 in both conditions (52). These investigators failedto detect the decrease in CMRO2 at altitude that had beenpredicted by Hochachka’s proposal of decreased metabolic rateas a defense against hypoxia (26). CMRO2 was also not alteredby 3.5 days at 3,810 m, �3.0 ml O2 �100 g�1 �min�1 (64).
CONCLUSIONS AND SUMMARY
Exposure to mild hypoxia rapidly induces an acute increasein CBF that becomes attenuated over 5 days as the oxygencarrying capacity of the blood increases. A later growth factordriven angiogenesis leads to increased capillary density over a2 wk interval, restoring tissue oxygen levels. The increased
ventilation rate is driven by the PO2 and stays elevated as longas PO2 stays low. CBF, probably controlled by brain stemsensors and circuits, responds to the oxygen carrying capacityof the blood. The microvasculature responds to tissue hypoxiawith transient angiogenesis. The delay between the fall inblood flow and the opening of new capillaries implies a periodof �1 wk or more during which the tissue is in uncompensatedhypoxia. It is unknown whether during this period normalneural function is affected or if there is a limit to the maximalwork rate of tissue until full tissue oxygen is restored. Bloodoxygen level-dependent functional magnetic resonance imag-ing studies in hypoxia-adapting subjects might prove revealingin this regard.
It remains to be determined whether or not these conclusionsapply to all species, including humans. For example, it wouldbe very useful to know whether there is a significant increasein blood volume that persists in humans adapting or adapted toaltitude. More definitive studies are needed in all species as towhether decreased metabolic rate contributes to hypoxic adap-tation.
GRANTS
This work has been supported by National Institutes of Health GrantsNS-38632 and GM-066309.
REFERENCES
1. Beall CM, Brittenham GM, Strohl KP, Blangero J, Williams-Blangero S, Goldstein MC, Decker MJ, Vargas E, Villena M, Soria R,Alarcon AM, and Gonzales C. Hemoglobin concentration of high-altitude Tibetans and Bolivian Aymara. Am J Phys Anthropol 106: 385–400, 1998.
2. Beck T and Krieglstein J. Cerebral circulation, metabolism, and blood-brain barrier in rats in hypocapnic hypoxia. Am J Physiol Heart CircPhysiol 252: H504–H512, 1987.
3. Bickler PE and Julian D. Regional cerebral blood flow and tissueoxygenation during hypocarbia in geese. Am J Physiol Regul Integr CompPhysiol 263: R221–R225, 1992.
4. Boero JA, Ascher J, Arregui A, Rovainen C, and Woolsey TA.Increased brain capillaries in chronic hypoxia. J Appl Physiol 86: 1211–1219, 1999.
5. Borgstrom L, Johannsson H, and Siesjo BK. The relationship betweenarterial PO2 and cerebral blood flow in hypoxic hypoxia. Acta PhysiolScand 93: 423–432, 1975.
6. Brown MM, Wade JPH, and Marshall J. Fundamental importance ofarterial oxygen content in the regulation of cerebral blood flow in man.Brain 108: 81–93, 1985.
7. Bryan RM Jr. Cerebral blood flow and energy metabolism during stress.Am J Physiol Heart Circ Physiol 259: H269–H280, 1990.
8. Chavez JC, Agani F, Pichiule P, and LaManna JC. Expression ofhypoxic inducible factor-1� in the brain of rats during chronic hypoxia.J Appl Physiol 89: 1937–1942, 2000.
9. Cohen PJ, Alexander SC, Smith TC, Reivich M, and Wollman H.Effects of hypoxia and normocarbia on cerebral blood flow and metabo-lism in conscious man. J Appl Physiol 23: 183–189, 1967.
10. Dahlgren N. Local cerebral blood flow in spontaneously breathing ratssubjected to graded isobaric hypoxia. Acta Anesthesiol Scand 34: 463–467, 1990.
11. Diemer K and Henn R. Kapillarvermehrung in der hirnrinde der ratteunter chronischem sauerstoffmangel. Die Natur 52: 135–136, 1965.
12. Drew KL, Harris MB, LaManna JC, Smith MA, Zhu XW, and MaYL. Hypoxia tolerance in mammalian heterotherms. J Exp Biol 207:3155–3162, 2004.
13. Dunn JF, Grinberg O, Roche M, Nwaigwe CI, Hou HG, and SwartzHM. Noninvasive assessment of cerebral oxygenation during acclimationto hypobaric hypoxia. J Cereb Blood Flow Metab 20: 1632–1635, 2000.
14. Dunn JF, Roche MA, Springett R, Abajian M, Merlis J, Daghlian CP,Lu SY, and Makki M. Monitoring angiogenesis in brain using steady-state quantification of DeltaR2 with MION infusion. Magn Reson Med 51:55–61, 2004.
Invited Review
728 CHRONIC HYPOXIA AND THE CEREBRAL CIRCULATION
J Appl Physiol • VOL 100 • FEBRUARY 2006 • www.jap.org

15. Edelman NH, Santiago TV, and Neubauer JA. Hypoxia and brain bloodflow. In: High Altitude and Man, edited by West JB and Lahiri S.Bethesda, MD: Am. Physiol. Soc., 1984, p. 101–113.
16. Faraci FM. Circulation during hypoxia in birds. Comp Biochem PhysiolA 85: 613–620, 1986.
17. Gilbert RD, Pearce WJ, and Longo LD. Fetal cardiac and cerebrovas-cular acclimatization responses to high altitude, long-term hypoxia. HighAlt Med Biol 4: 203–213, 2003.
18. Golanov EV, Christensen JR, and Reis DJ. Neurons of a limitedsubthalamic area mediate elevations in cortical cerebral blood flow evokedby hypoxia and excitation of neurons of the rostral ventrolateral medulla.J Neurosci 21: 4032–4041, 2001.
19. Golanov EV and Reis DJ. Contribution of oxygen-sensitive neurons ofthe rostral ventrolateral medulla to hypoxic cerebral vasodilation in the rat.J Physiol 495: 201–216, 1996.
20. Harik N, Harik SI, Kuo NT, Sakai K, Przybylski RJ, and LaMannaJC. Time course and reversibility of the hypoxia-induced alterations incerebral vascularity and cerebral capillary glucose transporter density.Brain Res 737: 335–338, 1996.
21. Harik SI, Behmand RA, and Arafah BM. Chronic hyperglycemiaincreases the density of glucose transporters in human erythrocyte mem-branes. J Clin Endocrinol Metab 72: 814–818, 1991.
22. Harik SI, Behmand RA, and LaManna JC. Hypoxia increases glucosetransport at blood-brain barrier in rats. J Appl Physiol 77: 896–901, 1994.
23. Harik SI, Hritz MA, and LaManna JC. Hypoxia-induced brain angio-genesis in the adult rat. J Physiol 485: 525–530, 1995.
24. Harik SI, Lust WD, Jones SC, Lauro KL, Pundik S, and LaMannaJC. Brain glucose metabolism in hypobaric hypoxia. J Appl Physiol 79:136–140, 1995.
25. Hochachka PW. Balancing conflicting metabolic demands of exerciseand diving. Fed Proc 45: 2948–2952, 1986.
26. Hochachka PW, Clark CM, Brown WD, Stanley C, Stone CK, NicklesRJ, Zhu GG, Allen PS, and Holden JE. The brain at high altitude:hypometabolism as a defense against chronic hypoxia? J Cereb BloodFlow Metab 14: 671–679, 1994.
27. Hochachka PW and Lutz PL. Mechanism, origin, and evolution ofanoxia tolerance in animals. Comp Biochem Physiol B Biochem Mol Biol130: 435–459, 2001.
28. Hudak ML, Koehler RC, Rosenberg AA, Traystman RJ, and JonesMD Jr. Effect of hematocrit on cerebral blood flow. Am J Physiol HeartCirc Physiol 251: H63–H70, 1986.
29. Iwamoto J, Curran-Everett DC, Krasney E, and Krasney JA. Cerebralmetabolic and pressure-flow responses during sustained hypoxia in awakesheep. J Appl Physiol 71: 1447–1453, 1991.
30. Jensen JB, Wright AD, Lassen NA, Harvey TC, Winterborn MH,Raichle ME, and Bradwell AR. Cerebral blood flow in acute mountainsickness. J Appl Physiol 69: 430–433, 1990.
31. Jones MD Jr, Traystman RJ, Simmons MA and Molteni RA. Effectsof changes in arterial O2 content on cerebral blood flow in the lamb. Am JPhysiol Heart Circ Physiol 240: H209–H215, 1981.
32. Julien-Dolbec C, Tropres I, Montigon O, Reutenauer H, Ziegler A,Decorps M, and Payen JF. Regional response of cerebral blood volumeto graded hypoxic hypoxia in rat brain. Br J Anaesth 89: 287–293, 2002.
33. Kety SS and Schmidt CF. The determination of cerebral blood flow inman by the use of nitrous oxide in low concentrations. Am J Physiol 143:53–66, 1945.
34. Kety SS and Schmidt CF. The effects of altered arterial tensions ofcarbon dioxide and oxygen on cerebral blood flow and cerebral oxygenconsumption of normal young men. J Clin Invest 27: 484–492, 1948.
35. Kety SS and Schmidt CF. The nitrous oxide method for the quantitativedetermination of cerebral blood flow in man: theory, procedure and normalvalues. J Clin Invest 27: 476–483, 1948.
36. Kissen I and Weiss HR. Cervical sympathectomy and cerebral micro-vascular and blood flow responses to hypocapnic hypoxia. Am J PhysiolHeart Circ Physiol 256: H460–H467, 1989.
37. Krasney JA, Jensen JB, and Lassen NA. Cerebral blood flow does notadapt to sustained hypoxia. J Cereb Blood Flow Metab 10: 759–764,1990.
38. Kreisman NR, Sick TJ, LaManna JC, and Rosenthal M. Local tissueoxygen tension-cytochrome a,a3 redox relationships in rat cerebral cortexin vivo. Brain Res 218: 161–174, 1981.
39. LaManna JC, Chavez JC, and Pichiule P. Structural and functionaladaptation to hypoxia in the rat brain. J Exp Biol 207: 3163–3169, 2004.
40. LaManna JC, Vendel LM, and Farrell RM. Brain adaptation to chronichypobaric hypoxia in rats. J Appl Physiol 72: 2238–2243, 1992.
41. Lauro KL and LaManna JC. Adequacy of cerebral vascular remodelingfollowing three weeks of hypobaric hypoxia. Examined by an integratedcomposite analytical model. Adv Exp Med Biol 411: 369–376, 1997.
42. Lenfant C and Sullivan K. Adaptation to high altitude. N Engl J Med284: 1298–1309, 1971.
43. Leniger-Follert E, Lubbers DW, and Wrabetz W. Regulation of localtissue PO2 of the brain cortex at different arterial O2 pressures. PflugersArch 359: 81–95, 1975.
44. Llanos AJ, Riquelme RA, Sanhueza EM, Hanson MA, Blanco CE,Parer JT, Herrera EA, Pulgar VM, Reyes RV, Cabello G, andGiussani DA. The fetal llama versus the fetal sheep: different strategies towithstand hypoxia. High Alt Med Biol 4: 193–202, 2003.
45. Longo LD, Hull AD, Long DM, and Pearce WJ. Cerebrovascularadaptations to high-altitude hypoxemia in fetal and adult sheep. Am JPhysiol Regul Integr Comp Physiol 264: R65–R72, 1993.
46. Lubbers DW and Baumgartl H. Heterogeneities and profiles of oxygenpressure in brain and kidney as examples of the PO2 distribution in theliving tissue. Kidney Int 51: 372–380, 1997.
47. Manohar M, Parks CM, Busch M, and Bisgard GE. Bovine regionalbrain blood flow during sojourn at a simulated altitude of 3500 m. RespirPhysiol 58: 111–122, 1984.
48. Meier P and Zierler KL. On the theory of the indicator dilution methodfor measurement of blood flow and volume. J Appl Physiol 6: 731–744,1954.
49. Metzger H, Erdmann W, and Thews G. Effect of short periods ofhypoxia, hyperoxia, and hypercapnia on brain O2 supply. J Appl Physiol31: 751–759, 1971.
50. Milledge JS and Sorensen SC. Cerebral arteriovenous oxygen differencein man native to high altitude. J Appl Physiol 32: 687–689, 1972.
51. Miller AT Jr and Hale DM. Increased vascularity of brain, heart, andskeletal muscle of polycythemic rats. Am J Physiol 219: 702–704, 1970.
52. Moller K, Paulson OB, Hornbein TF, Colier WN, Paulson AS, RoachRC, Holm S, and Knudsen GM. Unchanged cerebral blood flow andoxidative metabolism after acclimatization to high altitude. J Cereb BloodFlow Metab 22: 118–126, 2002.
53. Musch TI, Dempsey JA, Smith CA, Mitchell GS, and Bateman NT.Metabolic acids and [H�] regulation in brain tissue during acclimatizationto chronic hypoxia. J Appl Physiol 55: 1486–1495, 1983.
54. Nakai M, Iadecola C, Ruggiero DA, Tucker LW, and Reis DJ.Electrical stimulation of cerebellar fastigial nucleus increases cerebralcortical blood flow without change in local metabolism: evidence for anintrinsic system in brain for primary vasodilation. Brain Res 260: 35–49,1983.
55. Nilsson GE and Lutz PL. Anoxia tolerant brains. J Cereb Blood FlowMetab 24: 475–486, 2004.
56. Opitz E. Increased vascularization of the tissue due to acclimatization tohigh altitude and its significance for the oxygen transport. Exp Med Surg9: 389–403, 1951.
57. Patt S, Sampaolo S, Theallier-Janko A, Tschairkin I, and Cervos-Navarro J. Cerebral angiogenesis triggered by severe chronic hypoxiadisplays regional differences. J Cereb Blood Flow Metab 17: 801–806,1997.
58. Phillis JW. Adenosine and adenine nucleotides as regulators of cerebralblood flow: roles of acidosis, cell swelling, and KATP channels. Crit RevNeurobiol 16: 237–270, 2004.
59. Pichiule P, Chavez JC, and LaManna JC. Hypoxic regulation ofangiopoietin-2 expression in endothelial cells. J Biol Chem 279: 12171–12180, 2004.
60. Pichiule P and LaManna JC. Angiopoietin-2 and rat brain capillaryremodeling during adaptation and deadaptation to prolonged mild hyp-oxia. J Appl Physiol 93: 1131–1139, 2002.
61. Roy CS and Sherrington CS. On the regulation of the blood-supply ofthe brain. J Physiol 11: 85–108, 1890.
62. Schmidt-Nielsen K. Animal Physiology: Adaptation and Environment.New York: Cambridge University Press, 1983.
63. Schmidt-Nielsen K. Scaling: Why Is Animal Size So Important. NewYork: Cambridge University Press, 1984.
64. Severinghaus JW, Chiodi H, Eger EI, Brandstater B, and HornbeinTF. Cerebral blood flow in man at high altitude. Circ Res 19: 274–282,1966.
Invited Review
729CHRONIC HYPOXIA AND THE CEREBRAL CIRCULATION
J Appl Physiol • VOL 100 • FEBRUARY 2006 • www.jap.org

65. Shockley RP and LaManna JC. Determination of rat cerebral cortical bloodvolume changes by capillary mean transit time analysis during hypoxia,hypercapnia, and hyperventilation. Brain Res 454: 170–178, 1988.
66. Sick TJ, Lutz PL, LaManna JC, and Rosenthal M. Comparative brainoxygenation and mitochondrial redox activity in turtles and rats. J ApplPhysiol 53: 1354–1359, 1982.
67. Sorensen SC, Lassen NA, Severinghaus JW, Coudert J, and ZamoraMP. Cerebral glucose metabolism and cerebral blood flow in high-altituderesidents. J Appl Physiol 37: 305–310, 1974.
68. Underwood MD, Iadecola C, and Reis DJ. Lesions of the rostralventrolateral medulla reduce the cerebrovascular response to hypoxia.Brain Res 635: 217–233, 1994.
69. West JB. High Life: A History of High-Altitude Physiology and Medicine.New York: Oxford University Press, 1998.
70. Wolff CB. Cerebral blood flow and oxygen delivery at high altitude. HighAlt Med Biol 1: 33–38, 2000.
71. Wolff CB, Barry P, and Collier DJ. Cardiovascular and respiratoryadjustments at altitude sustain cerebral oxygen delivery—Severinghausrevisited. Comp Biochem Physiol A 132: 221–229, 2002.
72. Wolff HG. The cerebral circulation. Physiol Rev 16: 545–596, 1936.73. Wright BM. Apparatus for exposing animals to reduced atmospheric
pressure for long periods. Br J Haematol 10: 75–77, 1964.74. Xu K, Puchowicz MA, and LaManna JC. Renormalization of regional
brain blood flow during prolonged mild hypoxic exposure in rats. BrainRes 1027: 188–191, 2004.
75. Yang SP, Bergo GW, Krasney E, and Krasney JA. Cerebral pressure-flow and metabolic responses to sustained hypoxia: effect of CO2. J ApplPhysiol 76: 303–313, 1994.
Invited Review
730 CHRONIC HYPOXIA AND THE CEREBRAL CIRCULATION
J Appl Physiol • VOL 100 • FEBRUARY 2006 • www.jap.org