Administración_001
-
Upload
jose-luis-haro-vera -
Category
Documents
-
view
228 -
download
0
Transcript of Administración_001
-
8/3/2019 Administracin_001
1/11
Correspondence to C. Carpn (Tel.: +33 561 32 56 36; Fax. +33 561 32 56 23; e-mail: carpene@toulouse.
inserm.fr).
Influence of acute and chronic administration ofbenzylamine on glucose tolerance in diabetic and
obese mice fed on very high-fat diet
Z. Iffi-Soltsz1, 2, D. Prvot1, S. Grs1, S. Bour1, E. Szk2, C. Knauf3,R. Burcelin3, A. Fernndez-Quintela4, A. Lomba5, F. I. Milagro5 and C. Carpn1
1INSERM U858, IFR 31 Rangueil, I2MR, quipe 3, Universit Toulouse IIIPaul-Sabatier, Toulouse, France, 2Department of Pharmacodynamics, Semmelweis
University, Budapest, Hungary,3
INSERM U858, IFR 31 Rangueil, I2MR, quipe 2,Toulouse, France, 4Department of Nutrition and Food Science,University of Pas Vasco, Vitoria, Spain, 5Department of Nutrition, Food Science,
Physiology and Toxicology, University of Navarra, Pamplona, Spain
(Received on October, 2007)
Z. IFFI-SOLTSZ, D. PRVOT, S. GRS, S. BOUR, E. SZK, C.KNAUF, R. BURCELIN, A. FERNNDEZ-QUINTELA, A. LOMBA, F. I.MILAGRO and C. CARPN. Influence of acute and chronic administration of
benzylamine on glucose tolerance in diabetic and obese mice fed on very high-fat diet.J. Physiol. Biochem., 63 (4), 305-316, 2007.
The combination of vanadate plus benzylamine has been reported to stimulateglucose transport in rodent adipocytes and to mimic other insulin actions in diversestudies. However, benzylamine alone activates glucose uptake in human fat cells andincreases glucose tolerance in rabbits. The aim of this work was to unravel the ben-zylamine antihyperglycemic action and to test whether its chronic oral administra-tion could restore the defective glucose handling of mice rendered slightly obese anddiabetic by very high-fat diet (VHFD). When VHFD mice were i.p. injected withbenzylamine at 0.7 to 700 mol/kg before glucose tolerance test, they exhibited
reduced hyperglycemic response without alteration of insulin secretion. Whole bodyglucose turnover, as assessed by the glucose isotopic dilution technique, wasunchanged in mice perfused with benzylamine (total dose of 75 mol/kg). Howev-er, their in vivo glycogen synthesis rate was increased. Benzylamine appeared there-fore to directly facilitate glucose utilisation in peripheral tissues. When given chron-ically at 2000 or 4000 mol/kg/d in drinking water, benzylamine elicited a slightreduction of water consumption but did not change body weight or adiposity anddid not modify oxidative stress markers. Benzylamine treatment improved glucose
J. Physiol. Biochem., 63 (4), 305-316, 2007
-
8/3/2019 Administracin_001
2/11
tolerance but failed to normalize the elevated glucose fasting plasma levels of VHFDmice. There was no influence of benzylamine ingestion on lipolytic activity, basal andinsulin-stimulated glucose uptake, and on inflammatory adipokine expression in
adipocytes. The improvement of glucose tolerance and the lack of adverse effects onadipocyte metabolism, reported here in VHFD mice allow to consider orally givenbenzylamine as a potential antidiabetic strategy which deserves to be further studiedin other diabetic models.
Key words: Adipocyte, Semicarbazide-sensitive amine oxidase, Diabetes, Obesity.
Benzylamine is an alkaloid also namedmoringine and found in several medicinalplants (3) which, once ingested, can be
metabolized by semicarbazide-sensitiveamine oxidase (SSAO) and to a lesserextend by monoamine oxidase-B (MAO-B). Like other amine oxidase substrates,benzylamine generates hydrogen peroxidewhen oxidized. Among the end-productsof amine oxidation, hydrogen peroxide isknown to activate glucose transport andmetabolism, especially in adipocytes (10),while ammoniac and aldehydes are devoid
of such effects (11). Benzylamine has beenfirst reported to increase glucose transportand inhibit lipolysis in rat adipocytes inthe presence of vanadate (8, 19). The syn-ergism between benzylamine and vana-date is a consequence of the chemicalinteraction between the transition metaland hydrogen peroxide, which generatesperoxovanadate, an irreversible inhibitorof tyrosine phosphatases and a potentinsulin mimicker (2). Accordingly, all the
effects of vanadate plus benzylamine wereinhibited by antioxidants or by SSAOinhibitors (8). The insulin mimicry of ben-zylamine plus vanadate also functions invivo since they exert antidiabetic proper-ties, when subcutaneously injected incombination, or when continuously deliv-ered by implanted osmotic minipumps(1), or even when administered in theform of a complex salt (9). However, ben-
zylamine has been reported to exert
Z. IFFI-SOLTSZ, D. PRVOT, S. GRS, S. BOUR et al.306
J. Physiol. Biochem., 63 (4), 2007
diverse insulin-like effects by itself, with-out need for vanadate, such as stimulationof glucose transport and inhibition of
lipolysis in human fat cells (13), adipogen-esis in murine preadipocytes (17), andimprovement of glucose tolerance in con-scious rabbits and in obese mice (12).Moreover, we have recently reported thatchronic oral administration of benzy-lamine to normoglycemic non obese ratswas able to reduce their hyperglycemicresponse to a glucose load (5). The aim ofthe study was therefore to test whether
oral benzylamine administration was ableto improve glucose tolerance in a diabeticmodel. We take advantage of the mice ren-dered slightly obese and diabetic by veryhigh fat diet (VHFD) feeding (6) in whichwe have previously observed that benzy-lamine was able to acutely improve glu-cose tolerance in a manner that was inhib-ited by semicarbazide, a prototypicalSSAO inhibitor (12). The VHFD micewere therefore used to further study invivo the mechanism of action of benzy-lamine and to investigate whether chronicoral administration of benzylamine couldelicit beneficial actions on metabolic con-trol. Since sustained hydrogen peroxidegeneration by SSAO was the primaryeffect expected from benzylamine admin-istration, it was also verified whethercomplications of oxidative stress such aslipid peroxidation, protein glycation, adi-
pose tissue inflammation, or even alter-
-
8/3/2019 Administracin_001
3/11
ation in the expression of nitric oxide syn-thases or amine oxidases occurred in ben-zylamine-receiving VHFD-fed mice.
Another suspected adverse effect of givingbenzylamine in drinking water, alreadyreported in our preliminary study on rats,consisted in a small but consistent reduc-tion of water intake, probably due to thefact that high concentrations of benzy-lamine have a somewhat disgusting smell(5). Experiments were therefore conduct-ed with two benzylamine dosages, focus-ing attention to water consumption.
The following data show that, in mice
rendered obese and glucose intolerant bythree months of VHFD feeding, benzy-lamine dose-dependently reduced thehyperglycemic excursion in the glucosetolerance test, without modifying thepeak of insulin secretion. Increased glu-cose clearance was probably due to directstimulation of glycogen synthesis asfound in experiments conducted in vivowith labeled glucose. The antihyper-
glycemic action of benzylamine wasfound either after its acute injection orprolonged oral administration. The higheroral dose ingested (4000 mol/kg/day)slightly reduced water consumption butdid not affect body weight gain, adiposityor marker of oxidative stress or inflamma-tory response of adipose tissue. Sustainedingestion of benzylamine did not alter theexpression of amine oxidases inadipocytes, which exhibited unalteredlipolytic and glucose transport activities.
Material and Methods
Chemicals. Benzylamine hydrochlo-ride, bovine insulin, fatty-acid-free bovineserum albumin, and other reagents wereobtained from Sigma-Aldrich (SaintQuentin Fallavier, France). Enzymes for
glycerol assay and liberase blendzyme 3
were from Roche Diagnostics (Indianapo-lis, USA). 2-[1,2-3H]-deoxyglucose(2-DG, 29.7 Ci/mmol) and [3-3H]-glu-
cose were purchased from Perkin ElmerLife Science Products (Boston, USA).Ultrasensitive Insulin ELISA kit wasobtained from Mercodia (Uppsala, Swe-den), NEFA C Wako Free fatty acid(FFA) kit was from Oxoid (Dardilly,France) and lipid peroxidation markerswere determined with a kit from Oxitek(Bruxelles , Belgium).
Animals and treatments. C57Bl6 malemice were purchased from Charles Riverand (lArbresle, France) housed at 4-6 ani-mals per cage with free access to food andwater. For the first descriptive experi-ments, one group of 15 mice receivedstandard rodent chow while other groupof 45 mice was fed on very high fat diet(VHFD) containing, as percentage ofenergy content: 72 % fat (corn oil andlard), 28 % protein, and < 1 % carbohy-drate) (Safe, Augy, France). As previouslyreported, VHFD can produce in C57Bl6mice diverse states of obesity and/or dia-betes (6).
For studies on chronic effects of benzy-lamine on glycemic control and oxidativestress, mice turned on VHFD for at leastthree months were screened by intraperi-toneal glucose tolerance test (IPGTT) andonly those presenting glucose intolerance
were used for further studies. Two sets of32 VHFD-fed mice were separated in twogroups of equivalent body weight andhyperglycemic response to IPGTT. 16mice were fed VHFD without any addi-tional treatment (control), and their waterconsumption was determined weekly. 16other mice under VHFD were given ben-zylamine 4000 moles/kg/day in thedrinking water for 12 weeks (BZA-treat-
ed). BZA amount (in mg) to be dissolved
ORAL BENZYLAMINE AND GLUCOSE HANDLING 307
J. Physiol. Biochem., 63 (4), 2007
-
8/3/2019 Administracin_001
4/11
in 400 ml drinking solution was weeklyadjusted from mouse body mass (in g) anddaily water intake (in ml), according to the
formula: mg BZA = body mass/waterintake x 229.76. Typically, for miceweighing 31.5 g and drinking 4.4 ml/day,1645 mg BZA were dissolved in 400 mlwater and the bottles changed every week.Lastly, two other groups of VHFD wereconstituted in a similar manner: 12 VHFDcontrol and 12 VHFD drinking 2000moles of benzylamine/kg/day.
Intraperitoneal glucose tolerance tests
(IPGTT). Fasted mice (5 h) were i.p.injected with saline or benzylamine (0.7 to700 mol/kg) 15 min before i.p. glucose(1 g/kg) load. Blood was collected fromthe tail vein of conscious mice 0, 15, 30,45, 60, 90 and 120 min later for determi-nation of glucose levels with a glucoseme-ter (Roche Diagnostic, Mannheim, D).Blood was also collected before any i.p.injection to determine basal glycemia.
Area under the curve (AUC) of hyper-glycemic excursion was calculated andexpressed in arbitrary units as previouslydetailed (14).
Glucose turnover studies. A catheterwas indwelled into the femoral vein underanaesthesia, sealed under the back skin,and glued on the top of the skull. Themice were housed individually andallowed to recover for 4 days. Whole-
body glucose utilization rate was deter-mined in basal conditions in 6-hour fastedconscious mice. In basal state, D-[3H]3-glucose was continuously infused throughthe femoral vein at a rate of 10Ci/kg/min for 3 hours. Benzylamine wasalso continuously infused in a group ofmice of same body mass (32 g) at a ratereaching a total of 75 mol/kg at the endof the 2-hour experiment. Plasma glucose
concentrations and D-[3
H]3-glucose spe-
cific activity were determined in 5 l ofblood sampled from the tip of the tail veineach 10 minutes during the last hour of
infusion. Throughout the infusion period,blood samples (2.5 l) were collectedfrom the tip of the tail vein to assessglycemia. Calculations of glucoseturnover and of glycolysis and glycogensynthesis rates, based on the [3H]-H2Oappearance, were contucted as previouslydetailed (6).
Plasma and tissue sampling; lipolysisand glucose uptake in adipocytes. When
mice were sacrificed at the end of treat-ment, tissues and plasma were immediate-ly frozen for determination of diagnosticparameters using the above mentionedkits. Fluorometric analysis of circulatingadvanced-glycation end products (AGEs)was performed as previously reported(15). Internal white adipose tissues(perirenal plus retroperitoneal plus epi-didymal fat pads) were used for adipocyte
isolation and subsequent determination oflipolysis (by measurement of glycerolrelease) and 2-deoxyglucose uptake(2-DG), as previously described (13). Aportion of adipocytes was used for RNAisolation and real-time PCR experimentsas already detailed (4). Liver biopsies weresimilarly treated for gene expressionanalysis. Aortas were used for the deter-mination of nitrate/nitrite content by acapillary electrophoresis method accord-
ing to (18).
Statistical analysis. Results are given asmeans SEM and were compared usingStudents t test.
Results
Diabetes, hyperlipidemia and oxidativestress of VHFD-fed mice. Mice were fed
Z. IFFI-SOLTSZ, D. PRVOT, S. GRS, S. BOUR et al.308
J. Physiol. Biochem., 63 (4), 2007
-
8/3/2019 Administracin_001
5/11
a VHFD for three months before receiv-ing benzylamine acute injections or oralchronic administration. At this stage, they
were 17-week old, hyperglycemic (plasmaglucose: 8.27 0.33 vs. 6.60 0.22mM, n = 16, p< 0.001), hyperlipidemic(plasma unesterified fatty acids: 0.57 0.09 vs. 0.23 0.02 mM, p< 0.02), andmildy obese when compared to controlmice fed a standard diet. However, theywere not hyperinsulinemic (23 2 vs. 19 3 IU/ml, NS) since they ingested onlyvery limited amount of carbohydrates,practically absent in the VHFD. Never-theless, the glucose intolerant state ofVHFD mice was readily evidenced duringIPGTT: their hyperglycemic responsewas exaggerated when compared to con-trol (respective AUC was 920 28 vs.628 17 arbitrary units, p< 0.001). Onceinstalled, glucose intolerance remainedconstant for at least 3 months (not shown)and was concomitant with an increase inplasma markers of lipid peroxidation such
as malondialdehyde plus 4-hydroxy-2-nonenal (2.9 0.4 vs. 1.6 0.2 M, n =16, p< 0.02).
Beneficial effects of acute benzylamineadministration on glucose handling.Bolus i.p. injection of benzylamine didnot lower blood glucose in fasting VHFDmice which was 9.2 0.5 mM 15 minafter saline bolus, and remained at 8.7
0.3, 9.5 0.5, 8.5 0.5 and 9.1 0.2mM in mice receiving 0.7, 7, 70 and 700mol/kg benzylamine, respectively (NS).However, benzylamine greatly improvedglucose tolerance since it dose-dependent-ly reduced the hyperglycemic responseafter an i.p. glucose load (Fig. 1). The anti-hyperglycemic action of benzylamineoccurred without detectable change in theincrease of insulin plasma levels which
were identical 15 min after glucose load in
control and in mice receiving 7 mol/kgbenzylamine (not shown). Thisdemostrated that stimulation of insulin
secretion was not the main mechanism bywhich benzylamine exerted its antihyper-glycemic effect, and was in agreementwith the already reported lack of benzy-lamine action on isolated pancreatic islets(12).
It was tested whether the response to 7mol/kg benzylamine could be potentiat-ed by simultaneous administration ofvanadate. However no greater antihyper-glycemic effect was found when benzy-
lamine 7 mol/kg was associated withvanadate 22 mol/kg (respective AUC ofIPGTT were 469 38 and 441 35arbitrary units, n = 10-14, NS).
Fig. 2 shows that in vivo glucoseturnover, which is the balance betweenhepatic glucose production and wholebody glucose utilization, was not modi-fied by benzylamine in conscious VHFDmice. In the tissues, glucose can undergo
glycolysis or can be used for glycogen
ORAL BENZYLAMINE AND GLUCOSE HANDLING 309
J. Physiol. Biochem., 63 (4), 2007
Fig. 1. Dose-dependent effect of benzylamine on pro-voked hyperglycemic responses in VHFD mice.After 5-hour fasting, mice i.p. injected with saline (0)or the indicated dose of benzylamine 15 min beforeIPGTT consisting of a load of glucose at time 0
(1 g/kg, i.p.). Blood samples were collected from thetail vein of conscious animals at min 120 for immedi-ate blood glucose assay. Areas under the curve(AUC) of the hyperglycemic responses wereexpressed in arbitrary units. Means SEM of 4 to 8mice per group. Different from control at:
*p .05, **p
-
8/3/2019 Administracin_001
6/11
synthesis. Only the latter metabolic path-way was significantly increased by benzy-lamine, likely as the result of a facilitatedglucose uptake in peripheral tissues,including skeletal muscles. Prolonged
benzylamine administration was thereforeperformed to test whether similar antihy-perglycemic effect of this amine could beobtained when orally administered atdoses of 2000 or 4000 mol/kg/day.
Water intake in VHFD mice drinkingbenzylamine. The average daily waterintake was 4.4 0.1 g in mice receivingthe higher dose of benzylamine (BZA-treated) while it was 4.8 0.1 g in mice
drinking only water (n = 16, p< 0.05).Reduction of water intake persisted alllong the 12-week treatment. It could notbe excluded that reduced consumption ofbenzylamine-containing solution was dueto an aversive effect of the amine, whichexhibits a disgusting smell at very highconcentrations. It was difficult to assesswhether this reduction of water intakewas concomitant with change in calorie
intake because the very high fat chow was
peculiarly sticky and did not facilitateaccurate determination of food consump-tion. Nevertheless, after 12 weeks of treat-ment, there was no difference in body
mass between the control and the BZA-treated groups, even at the higher dosetested. Similarly, there was not any changein adipose tissue, liver, or heart mass.
Influence of benzylamine chronic treat-ment on glucose tolerance. After threeweeks of treatment, mice treated or notwith benzylamine were fasted for 5 hoursand submitted to IPGTT (Fig. 3). The
overall hyperglycemic excursion wasreduced by BZA-treatment since the areasunder the curves presented in Figure 3were equivalent to 1088 52 and 911 58 arbitrary units in control and BZA-treated mice, respectively (n = 11, p
-
8/3/2019 Administracin_001
7/11
and BZA-treated mice, reaching a mini-mum of 6.0 0.2 and 6.7 0.3 mMwithin 30 min (n = 9, NS). Despite this
beneficial effect of benzylamine on glu-cose tolerance, fasting plasma glucose andinsulin were unchanged in BZA-treatedmice, even after benzylamine treatment at4000 mol/kg/day for 12 weeks (notshown). Surprisingly, glycemia was lowerin fed than in fasted state in VHFD miceand a significant beneficial effect of BZA-treatment was not observed under fedconditions at several time points of thetreatment. For instance, four weeks afterthe start of treatment, non-fasting boodglucose was 8.27 0.33 mM in controlVHFD and was lowered to 7.32 0.22mM in mice drinking benzylamine at 2000mol/kg (n = 12, p
-
8/3/2019 Administracin_001
8/11
unchanged after BZA-treatment, and that
combination of 0.1 mM benzylamineplus 0.1 mM vanadate clearly reproducedinsulin activation of hexose transport inadipocytes from both VHFD control andBZA-treated mice. Therefore, no alter-ation of the adipocyte responses to insulinor to insulin mimicking agents could bedetected after benzylamine oral adminis-tration.
Discussion
Taken together, these results show thatbenzylamine acutely facilitates glucosedisposal. When added into the drinkingwater, it did not dramatically impair waterand food consumption since it did notalter body weight gain of VHFD mice.Chronic benzylamine ingestion wasdevoid of adverse effects on nitric oxide
bioavailability in the vasculature or on
markers of inflammation in the adiposedepots while it improved several indexesof glucose homeostasis.
Our results perfectly confirm the find-ings of a preliminary experiment per-formed with Wistar rats showing that oraladministration of benzylamine (1870mol/kg/day) did not decrease of foodand water consumption (5). Moreover,they reproduced our observation of thebenefits of orally given benzylamine onglucose handling to diabetic monse modelby VHFD feeding. In fact, it has been
recently reported that VHFD micerespond to a single injection of hexa-quis(benzylammonium) decavanadate,which is a complex salt of vanadium andbenzylamine, by an improvement of glu-cose tolerance (9). Although the demon-stration of insulin-like actions of vanadateplus benzylamine is of interest, itremained to be clarified whether benzy-lamine alone is also able to act on a rodentmodel of diabetes for at least two reasons:
1) vanadium is potently toxic and, in spiteof increasing its bioavailability at the tar-gets of insulin mimicry, it may alter over-all phosphorus metabolism; 2) the pres-ence of vanadate does not improve theinsulin-like effects of benzylamine inhuman adipocytes (13) or murinepreadipocytes (7). Thus, it might be sus-pected that the synergism observedbetween the amine and the transition
metal in the diabetic models studied so farcould not be easily extrapolated to diabet-ic patients. In this context, it was justifiedto test whether a diabetic model shown invivo to be responsive to arylalkylaminevanadium salts could be influenced bybenzylamine alone. When the presentwork was initiated, it was only knownthat benzylamine alone at 0.1 mM wasable to elicit 11 2 % of the insulin in
vitro maximal stimulation of glucose
Z. IFFI-SOLTSZ, D. PRVOT, S. GRS, S. BOUR et al.312
J. Physiol. Biochem., 63 (4), 2007
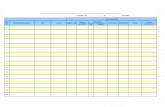
Fig. 4. Effect of benzylamine chronic treatment onadipocyte glucose uptake.
White adipocytes were incubated for 45 min with 10
and 100 nM insulin (ins) or with 0.1 and 1 mM ben-zylamine plus 0.1 mM vanadate (benz + van)before a 10-min hexose uptake assay with 2-DG.Means SEM of 6 mice per group. There was notsignificant difference between VHFD-fed control(black columns) and BZA-treated mice (opencolumns) while basal uptake was significantly stimu-lated in all the conditions tested: ***p
-
8/3/2019 Administracin_001
9/11
uptake in fat cells from VHFD mice,while its combination with 0.1 mM vana-date could reach up to 51 5 % of
insulin effect. However, 1 mM benzy-lamine could reproduce a quarter of theinsulin stimulation (12). Although mod-est, this activation obtained with benzy-lamine alone could be sufficient to partic-ipate to the restoration of impaired glu-cose tolerance, if continuously applied todiabetic VHFD mice.
VHFD mice clearly responded to ben-zylamine challenges by limiting theirhyperglycemic response during IPGTT.However, the chronic oral administrationdid not totally normalized the relativeglucose intolerance of VHFD mice since itdid not reduce their slightly increasedfasting glycemia. Decrease of blood glu-cose levels was observed only in fed statebut did not consistently appearedthroughout BZA-treatment. This wasprobably the consequence of the highvariability glycemia of fed animals, which
unexpectedly remained lower than in thefasted state. A possible explanation forthis peculiar glucose homeostasis is thatVHFD mice are starved from alimentaryglucose even under fed conditions sincetheir diet is devoid of carbohydrates.These mice which are intolerant to a glu-cose load do not display all the typical fea-tures of type 2 diabetes: they do notexhibit hyperinsulinemia and show lower
protein glyc(oxid)ation index (AGEs)than normoglycemic mice fed a controldiet. Therefore, it might be difficult for anagent deemed to favour glucose utilizationin peripheral tissues to correct the defectof VHFD mice which have practicallyhepatic neoglucogenesis as sole source ofglucose. This may explain the differencebetween the impressive beneficial actionof benzylamine on glucose handling in the
presence of a glucose load and its incon-
sistent action of fasting hyperglycemia inVHFD mice. This may also explain thediscrepancy with streptozotocin-induced
diabetic rats, the hyperglycemia of whichis not normalized but significantlyreduced by repeated s.c. administration ofbenzylamine alone (15). In the latter case,disposal of ingested glucose was impairedand gained to be improved by benzy-lamine. The benzylamine-dependent acti-vation of glucose transport, de novo lipo-genesis and glycogen synthesis are inagreement with this hypothesis. The lack
of effect of benzylamine on insulinresponse during IPGTT can also be inter-preted on the basis of in vitro experi-ments: benzylamine was unable to stimu-late insulin secretion in pancreatic isletsfrom VHFD-fed mice (M. J. Garca-Ba-rrado, personal communication). Sincebenzylamine hardly reduced the peak ofhyperglycaemic response to a glucoseload, but rather facilitated and shortenedthe return to basal values, it appears likely
that insulin release was unchanged duringthe first phase of IPGTT. In keeping withthis, the absence of change in the sensitiv-ity to hypoglycemic effect of insulin is inaccordance with the unaltered glucosetransporter equipment and insulinresponsiveness found in adipocytes fromBZA-treated mice. Continuous monitor-ing of the changes in plasma levels ofinsulin and glucose during clamp experi-
ments will considerably help in under-standing the benzylamine mechanism ofaction.
The sustained presence of benzylaminedid not elicit detectable deleterious effectson the vasculature, as it was the case formethylamine, another SSAO substratetested in transgenic mice overexpressingthe soluble form of SSAO (16). Takentogether, our results indicate that the
improvement of glucose tolerance
ORAL BENZYLAMINE AND GLUCOSE HANDLING 313
J. Physiol. Biochem., 63 (4), 2007
-
8/3/2019 Administracin_001
10/11
obtained in VHFD mice receiving benzy-lamine and the lack of detectable adverseeffects are not only confirmatory of previ-
ous works reporting insulin-like effects ofbenzylamine with or without vanadatebut can be considered as a preliminaryapproach necessary for further studies onthe oral antidiabetic properties of amineoxidase substrates. On the basis of thepresent findings, oral benzylamine admin-istration deserves to be tested on otherpharmacological, nutritional or geneticdiabetic models until the search for selec-tive amine oxidase substrates leads todetection of more powerful insulin mim-ickers suitable for clinical investigation.
Acknowledgements
This work was partly supported by Commu-naut de Travail des Pyrnes, by Balaton Pro-gramme of french-hungarian exchanges and by theHungarian National Office of Research and Tech-nology and the Agency for Research Fund Manage-ment and Research Exploitation. The authorsexpress gratitude to E. Wanecq, to the staff of PA3S(Toulouse) for facilitating scientific exchanges, andto T. Sulpice (Physiogenex, Labge) for invaluablehelp.
Z. IFFI-SOLTSZ, D. PRVOT, S.GRS, S. BOUR, E. SZK, C. KNAUF, R.BURCELIN, A. FERNNDEZ-QUINTE-LA, A. LOMBA, F. I. MILAGRO y C. CAR-PN. Influencia de la benzilamina en admi-nistracin aguda y crnica sobre la tolerancia ala glucosa en ratones diabticos y obesos ali-
mentados con dieta hipergrasa.J. Physiol. Bio-chem., 63 (4), 305-316, 2007.
Se ha descrito que la combinacin de vana-dato y benzilamina estimula el transporte deglucosa en los adipocitos de roedor y que pro-mueve otros efectos de tipo insulina. La benzi-lamina sola activa la captacin de glucosa enadipocitos humanos e incrementa la toleranciaa la glucosa en el conejo. En este trabajo, se hatratado de profundizar en la accin antihiper-
glucemiante de la benzilamina y a probar si su
administracin oral crnica poda normalizarla glucemia en ratones ligeramente obesos ydiabticos tras una dieta muy rica en grasa
(VHFD). Cuando la benzilamina se adminis-traba (i.p.; de 0,7 a 700 moles/kg) a ratonesVHFD antes de realizar el test de tolerancia ala glucosa, la respuesta hiperglucmica se redu-ca sin alterar la secrecin de insulina. Cuandolos ratones VHFD se perfundan con glucosaradiactiva, la benzilamina (dosis total de 75moles/kg) no cambi el turnoverde glucosapero aument la sntesis de glucgeno, facili-tando la utilizacin de glucosa en los tejidosperifricos. Cuando se administr crnicamen-
te a 2000 a 4000 moles/kg/da en el agua delbebedero, la benzilamina produjo una ligerareduccin del consumo de agua pero no cam-bi el peso corporal o la adiposidad y no modi-fic los marcadores de estrs oxidativo. Estetratamiento mejor la tolerancia a la glucosapero no fue capaz de normalizar los nivelesplasmticos en ayunas de glucosa en los rato-nes VHFD. Asimismo, no hubo influencia dela ingestin de benzilamina sobre la actividadlipoltica o la captacin de glucosa ni sobre la
expresin de adipoquinas inflamatorias en adi-pocitos. En suma, la mejora de la tolerancia a laglucosa y la falta de efectos adversos, observa-dos en ratones VHFD, permite considerar a labenzilamina administrada oralmente como unaestrategia antidiabtica potencial que requiereser estudiada en profundidad en otros modelosdiabticos.
Palabras clave: Adipocitos, Amino oxidasa sensiblea semicarbazida, Diabetes, Obesidad.
References
1. Abella, A., Marti, L., Camps, M., Claret, M., Fer-nandez-lvarez, J., Gomis, R., Gum, A.,Viguerie, N., Carpn, C., Palacin, M., Testar,X., Zorzano, A. (2003): Diabetes, 52, 1004-1013.
2. Abella, A., Marti, L., Carpn, C., Palacin, M.,Testar, X., Zorzano, A. (2003): J. Physiol.Biochem., 59, 153-160.
3. Anwar, F., Latif, S., Ashraf, M., Gilani, A.H.
(2007): Phytother. Res., 21, 1725.
Z. IFFI-SOLTSZ, D. PRVOT, S. GRS, S. BOUR et al.314
J. Physiol. Biochem., 63 (4), 2007
-
8/3/2019 Administracin_001
11/11
4. Bour, S., Daviaud, D., Gres, S., Lefort, C.,Prvot, D., Zorzano, A., Wabitsch, M., Saulnier-Blache, J.-S., Valet, P., Carpn, C. (2007):Biochimie, 89, 916-925.
5. Bour, S., Visentin, V., Prvot, D., Daviaud, D.,Saulnier-Blache, J.-S., Guign, C., Valet, P.,Carpn, C. (2005):J. Physiol. Biochem., 61, 371-379.
6. Burcelin, R., Crivelli, V., Dacosta, A., Roy-Tirelli, A., Thorens, B. (2002): Am. J. Physiol.Endocrinol. Metab., 282, E834-E842.
7. Carpn, C., Daviaud, D., Boucher, J., Bour, S.,Visentin, V., Grs, S., Duffaut, C., Fontana, E.,Testar, X., Saulnier-Blache, J.-S., Valet, P. (2006):Metabolism, 55, 1397-1405.
8. Enrique-Tarancn, G., Marti, L., Morin, N.,Liczano, J., Unzeta, M., Sevilla, L., Camps, M.,Palacin, M., Testar, X., Carpn, C., Zorzano, A.(1998):J. Biol. Chem., 273, 8025-8032.
9. Garca-Vicente, S., Yraola, F., Marti, L., Gonza-lez-Munoz, E., Garca-Barrado, M. J., Canto, C.,Abella, A., Bour, S., Artuch, R., Sierra, C., Bran-di, N., Carpn, C., Moratinos, J., Camps, M.,Palacin, M., Testar, X., Guma, A., Albericio, F.,Royo, M., Mian, A., Zorzano, A. (2007): Dia-betes, 56, 486-493.
10. Goldstein, B. J., Mahadev, K., Wu, X., Zhu, L.,Motoshima, H. (2005): Antioxid. Redox Signal.,7, 1021-1031.
11. Iglesias-Osma, M.C., Bour, S., Garca-Barrado,M. J., Visentin, V., Pastor, M. F., Testar, X.,Marti, L., Enrique-Tarancon, G., Valet, P.,Moratinos, J., Carpn, C. (2005): Pharmacol.
Res., 52, 475-484.12. Iglesias-Osma, M. C., Garca-Barrado, M. J.,Visentin, V., Pastor-Mansilla, M. F., Bour, S.,Prvot, D., Valet, P., Moratinos, J., Carpn, C.(2004):J. Pharmacol. Exp. Ther., 309, 1020-1028.
13. Morin, N., Lizcano, J. M., Fontana, E., Marti, L.,Smih, F., Rouet, P., Prvot, D., Zorzano, A.,Unzeta, M., Carpn, C. (2001): J. Pharmacol.Exp. Ther., 297, 563-572.
14. Morin, N., Visentin, V., Calise, D., Marti, L.,Zorzano, A., Testar, X., Valet, P., Fischer, Y.,Carpn, C. (2002): J. Pharmacol. Exp. Ther.,303, 1238-1247.
15. Soltesz, Z., Tabi, T., Halasz, A. S., Palfi, M., Koc-sis, E., Magyar, K., Toth, M., Szk, E. (2007):J.Neural Transm., 114, 851-855.
16. Stolen, C. M., Madanat, R., Marti, L., Kari, S.,Yegutkin, G. G., Sariola, H., Zorzano, A., Jalka-nen, S. (2004):FASEB J., 18, 702-704.
17. Subra, C., Fontana, E., Visentin, V., Testar, X.,Carpn, C. (2003):J. Physiol. Biochem., 59, 209-216.
18. Szk, E., Tabi, T., Halasz, A. S., Palfi, M., Mag-yar, K. (2004):J. Chromatogr. A., 1051, 177-183.
19. Visentin, V., Prvot, D., Marti, L., Carpn, C.(2003): Eur. J. Pharmacol., 466, 235-243.
ORAL BENZYLAMINE AND GLUCOSE HANDLING 315
J. Physiol. Biochem., 63 (4), 2007