GIST NIÑOS
-
Upload
juan-jose-leon -
Category
Documents
-
view
221 -
download
0
Transcript of GIST NIÑOS
-
8/12/2019 GIST NIOS
1/9
ORIGINALARTICLE
Gastrointestinal Stromal Tumors of the Stomachin Children and Young Adults
A Clinicopathologic, Immunohistochemical, and MolecularGenetic Study of 44 Cases With Long-Term Follow-Upand Review of the Literature
Markku Miettinen, MD,* Jerzy Lasota, MD,* and Leslie H. Sobin, MD
Abstract:Gastrointestinal stromal tumors (GISTs), specific KIT- orPDFGRA-signaling driven mesenchymal tumors, are rare in children
and young adults, and their clinicopathologic and molecular genetic
profile is incompletely understood. In this study, we analyzed 44 gas-
tric GISTs occurring by the age of 21 years. There were 32 females
and 12 males, youngest of whom were a 5-year-old boy and an
8-year-old girl. All but 1 of 25 patients under the age of 16 were girls.
The patients most commonly received medical attention because of
chronic, insidious gastrointestinal bleeding with anemia, less com-
monly with acute GI bleeding. Only 1 patient had Carney triad with
pulmonary chondroma. None of the patients had family members with
GIST. The tumors measured from 1.5 to 24 cm (median, 5.6 cm). A
total of 21 tumors with specified location were in the antrum and
8 were in the gastric body. Histologically, 26 tumors were composed
of epithelioid cells, 12 of spindle cells, and 6 of combination thereof.
Mitotic activity varied form 0 to 65/50 HPF (median, 5/50). All but
one of the 24 tumors tested were KIT-positive, and 20 were CD34-
positive. Eleven patients developed liver or abdominal metastases, and
6 of them died of tumor surviving 5.5 to 35.5 years (median, 16 years)
after the first surgery; three of these tumors had a low mitotic activity
and size ,10 cm. Twenty-one patients were alive with no evidence for
disease 7 to 41 years (median, 17 years) after the first surgery. None
of the 13 tumors examined (7 of them 8- to 16-year-old females) had
KIT exon 9, 11, 13, or 17 or PDGFRA exon 12 or 18 mutation as
typically seen in adult GISTs. Gastric GISTs in children have mainly
epithelioid morphology, often occur in antrum, and have a somewhat
unpredictable but slow course of disease. Their pathogenesis may differ
from that of adult GISTs because no KIT or PDGFRA mutations were
found; connection with Carney triad seems infrequent despite demo-
graphic and histologic similarities.
Key Words: gastrointestinal stromal tumor, stomach, child, prog-
nosis, KIT, PDGFRA, mutation
(Am J Surg Pathol 2005;29:13731381)
Gastric stromal tumors (GISTs), the specific KIT-positiveand KIT- or PDGFRA-driven mesenchymal tumors ofthe GI tract, typically occur in older adults and compriseapproximately 60% of all GISTs of all sites.37 Thesetumors seem to be very rare in children and young adults andare mostly reported in the English literature as singlecases and small series with scant data on long-termfollow-up.4,6,10,11,1315,2022,25,26,30,33,34,36,4244,4749,5254 Someof those tumors were reported as gastrointestinal autonomicnerve tumors (GANTs) currently understood as variants ofGIST, based on similar KIT expression and KIT mutations,31
and others as gastric leiomyomas, leiomyoblastomas, and
leiomyosarcomas. Some GISTs in children and young adultsoccur in connection with Carney triad or GIST paragangliomasyndrome, of which a large series was published, including ap-proximately 45 patients 20 years old or younger and showing arelatively indolent course of disease with commonly persistingdisease.7,8
A majority of adult GISTs have gain-of-function muta-tions in KIT or PDGFRA, two closely related receptor tyrosinekinases.16,17,24,27,46 However, there is little information on mu-tation status in GISTs at young age with only 1 case reportedand found to be KIT mutation negative.33 In this study, wepresent a clinicopathologic, immunohistochemical, and mo-lecular genetic analysis of 44 gastric GISTs in children andyoung adults, all but one of which occurred outside the setting
of Carney triad/GIST paraganglioma syndrome.
MATERIALS AND METHODS
Case MaterialAll cases coded as gastric smooth muscle or stromal
tumors (including any alternative designation) submitted fromthe United States or Canada during 1970 to 1996 (n = 1877)were retrieved. Of these 1877 tumors, 55 occurred at or underthe age of 21 years. Forty-four tumors were histologically
From the Departments of *Soft Tissue Pathology and Hepatic and Gastro-intestinal Pathology, Armed Forces Institute of Pathology, Washington, DC.
The opinions and assertions contained herein are the expressed views of theauthors and are not to be construed as official or reflecting the views of theDepartments of the Army or Defense.
Reprints: Markku Miettinen, MD, Department of Soft Tissue Pathology,Armed Forces Institute of Pathology, 6825 16th Street NW, Bldg 54, RmG090, Washington, DC 20306-6000 (e-mail: [email protected]).
Copyright 2005 by Lippincott Williams & Wilkins
Am J Surg Pathol Volume 29, Number 10, October 2005 1373
-
8/12/2019 GIST NIOS
2/9
classified as GISTs and included in this study. The classi-fication was based on the known histologic spectrum of KIT-positive gastric GISTs with spindle cell or epithelioid features,and with one exception, on KIT positivity. Based on reclas-sification, 11 tumors were excluded: 4 inflammatory myofi-broblastic tumors, 1 desmoid, 1 small round cell desmoplastictumor, 3 benign mesenchymal tumors not further classified,
and 2 unclassified sarcomas. There were no true leiomyomas,leiomyosarcomas, or schwannomas.
Clinical datawere reviewed from the records, and follow-upinformation was obtained from the hospital records, tumor reg-istries, primary care physicians, patients, or in some cases fromfamily members, according to the institutional review boardapproval.
For the purpose of clinicopathologic comparison, thegastric GISTs were divided into eight groups based on tumormaximum diameter and mitotic activity per 50 high powerfields (HPFs), as previously detailed.40 The groups were de-fined as follows: group 1, tumors 2 cm or less in diameter with5 or fewer mitoses per 50 HPF; group 2, tumors larger than 2 cmand not over 5 cm, with 5 or fewer mitoses per 50 HPF; group3a, tumors larger than 5 cm and not over 10 cm, with 5 or fewermitoses per 50 HPF; group 3b, tumors larger than 10 cm, with5 or fewer mitoses per 50 HPF; group 4, tumors 2 cm orsmaller and with more than 5 mitoses per 50 HPF; group 5,tumors larger than 2 cm and not over 5 cm and with more than5 mitoses per 50 HPF; group 6a, tumors larger than 5 cm andnot over 10 cm with more than 5 mitoses per 50 HPF; group6b, tumors larger than 10 cm with more than 5 mitoses per50 HPF.
Analysis of Histologic ParametersA total of 1 to 26 hematoxylin and eosin-stained slides
(median, 7 slides) were reviewed of each case. Mitotic figureswere counted in 50 fields by searching the most mitoticallyactive areas or until 100 mitoses were found. The total area ofthe 50 fields measured 5.3 mm2. The mitosis counting as wellas enumeration of histologic features was performed blindlywithout knowing tumor outcome.
The tumors were subclassified and histologic featuresenumerated as previously reported.40 By cell type, the tumorswere divided into spindle, epithelioid, or combination types.By subtype, the spindle cell tumors were divided into scle-rosing, palisaded- vacuolated, hypercellular, and sarcomatousones, and the epithelioid tumors were divided into sclerosing,discohesive, hypercellular, and sarcomatous subtypes. The fol-lowing additional parameters were recorded in all cases: nuclearatypia, presence of coagulative or liquefactive necrosis, mucosalinvasion, calcification, organoid pattern, nuclear palisading, andcytoplasmic vacuolization.
ImmunohistochemistryAll tumors with available paraffin blocks or unstained
slides were evaluated. The primary antibodies, sources, dilutions,and pretreatments were the following: CD34, clone QBEND/10,Biogenex, San Ramon, CA 1:40, Sigma protease VIII for2 minutes; KIT (CD117), polyclonal antibody A4502, 1:200(Dako, Carpinteria, CA) with heat-induced epitope retrieval byEDTA buffer; smooth muscle actin, clone 1A3 (Sigma, St.
Louis, MO, 1:50 no pretreatment); desmin, clone D33 (Dako1:50, heat-induced epitope retrieval by EDTA buffer); S-100protein, polyclonal (Dako, 1:1600, no pretreatment).
The primary antibodies were incubated 1 hour at roomtemperature. The detection was performed using the Envisionnon-avidin-biotin based polymer system (Dako) with diami-nobenzidine as the chromogen.
Molecular GeneticsDNAwas extracted from formalin-fixed, paraffin-embedded
tissue in 13 cases. Sequences of KIT exon 9, 11, 13, 17 andPDGFRA exon 12 and 18 were PCR-amplified and analyzedas previously described.2729
RESULTSA total of 44 patients with GISTs of age of 21 or under
were identified among 1782 patients with gastric GISTs (2.6%).There were 32 females and 12 males with age range 5 to21 years (median and mean, 14.5 years). Only 2 patients were
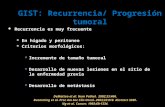
younger than 10 years: a 5-year-old boy and an 8-year-old girl.All but 1 patient under age 16 were female. The age and sexdistribution is shown in Figure 1.
Clinical FeaturesThe clinicopathologic features are summarized in Table 1.
A great majority of patients with known clinical history (35 of37 patients, 95%) presented with gastrointestinal bleeding. Thiswas most commonly insidious leading to anemia and relatedsymptoms such as syncope and weakness. Six patients werespecified to have hematemesis and 5 had melena, and 3 pa-tients had both. One patient had upper abdominal discomfortand another was diagnosed umbilical hernia caused by tumor.One patient had Carney triad. She had a gastric epithelioid
GIST first excised at the age of 12 years and had surgery forpulmonary chondroma 3 years later. The details of this patientwere reported previously.40 None of the patients had evidencefor paraganglioma, neurofibromatosis type I, or familial GIST;the information was based in addition to documents, interviewof 19 patients or family members.
FIGURE 1. Age and sex distribution of 44 gastric GISTs inchildren and young adults. Pale = males; dark = females.
1374 q 2005 Lippincott Williams & Wilkins
Miettinen et al Am J Surg Pathol Volume 29, Number 10, October 2005
-
8/12/2019 GIST NIOS
3/9
TABLE 1. Clinicopathologic Features of the 44 Children and Young Adults With a Gastric GIST
PatientNo.
Age(y r) Sex
Size(cm) Location
Mitoses/50 HPF
CellType
PrognosticGroup
Recurrences/Metastases(yrs from onset) Follow-Up (yrs) Outcome
1 5 M 14.5 Anterior wall 0 E 3b
2 8 F 8 LC 18 E 6a Abdominal mets, 18 18 AWD
3 10 F 5 LC 10 E 5
4 10 F 5.7 3 E 3a 8.6 ANED5 10 F .10 LC 8 E 6b Gastric recurrence, 13,
gastrectomy29.4 ANED
6 10 F ND Cardia, posterior wall
14 (met) E Liver mets, durationunknown
35.5 DOD
7 11 F 3 Antrum 16 E/S 5
8 11 F 5 0 E 2 7 ANED
9 11 F 5 Antrum, LC 3 E 2
10 11 F 6 Antrum, posterior wall 37 S 6a Liver mets, 4.5 5.6 DOD
11 11 F 7 Antrum, near LC 16 E 6a
12 12 F 2.7 LC 6 S 5
13 12 F 5 Antrum, LC 18 E 5 Gastric recurrences, 9 and 30,total gastrectomy
41.2 ANED
14 12 F 6 Distal 2 E 3b Liver mets, 4.5 8.9 AWD
15 12 F 8.5 LC 7 E 6a Liver mets,at presentation
AWD
16 13 F 4.3 Fundus, LC, post wall 4 S 2 Liver mets, time of diagnosis unknown
6.5 DOD
17 13 F .10 Distal, GC 11 E 6b Liver mets, 14 20.4 DOD
18 14 F 3.5 LC 2 E 2 28 ANED
19 14 F 4.5 Upper body 7 E 5 13 ANED
20 14 F 6 LC 4 E/S 3a 20.7 ANED
21 14 F 6 Antrum, posterior wall 1 E 3a Liver mets, 7 21.5 AWD
22 14 F 7 Antrum, LC 1 E/S 3a 27.5 ANED
23 14 F 9 Antrum 6 S 6a
24 15 F 3.5 Antrum, fundus,multiple
6 E/S 5 8.1 ANED
25 15 F 24 Distal stomach 65 E 6b Abdominal and liver mets, 4 11 DOD
26 16 F 1.5 Antrum 1 E
27 16 M 4 Antrum, LC 9 S 5 10.8 ANED28 16 M 8 2 E 3a Liver mets, 22 23.3 DOD
29 17 M 2.7 6 S 5 Liver mets, 11 11.3 AWD
30 17 M 4 Antrum, LC 2 E 2 17.3 ANED
31 17 M 5 Antrum, LC 30 S 5 31.2 ANED
32 18 F 3.5 3 E/S 2
33 18 F 5.5 Distal, posterior wall 2 S 3a
34 18 M ND Cardia, posterior wall 7 E 12.2 ANED
35 19 F 1.5 Antrum 4 E 2 17.5 ANED
36 19 F 6.5 Antrum, anterior wall 16 S 6a
37 19 F 12 Posterior wall 3 E 3b 16.6 ANED
38 19 M 3.8 Distal body 0 E 2
39 19 M 5 Fundus 15 S 5 29.3 ANED
40 19 M 6 Antrum 12 E 6a 14.7 ANED
41 20 M 7 GC, anterior 3 S 3a 34.2 ANED
42 21 F 3.5 Antrum 0 S 2 7.4 ANED
43 21 F 7 Body 13 E/S 6a 10.1 ANED
44 21 M 7 Mid-body 2 E 3a multiple 17.3 ANED
LC, lesser curvature; GC, great curvature; ANED, alive with no evidence of disease; AWD, alive with disease; DOD, dead of disease; mets, metastases.
q 2005 Lippincott Williams & Wilkins 1375
Am J Surg Pathol Volume 29, Number 10, October 2005 Gastric GISTs in Children
-
8/12/2019 GIST NIOS
4/9
A majority of the tumors with specified location occurredin the antrum (n = 21). Eight tumors were known to occur inthe gastric body (3 in fundus, 2 in cardia, and 3 elsewhere). Atleast 2 patients had multiple tumors: 1 (patient no. 24, Table 1)had two tumors: one in the antrum and another in the fundus,and another (patient no. 44, Table 1) had multiple tumornodules in gastric body. In addition, four tumors were grossly
multinodular, probably representing a single tumor in one regionof the stomach.
The types of primary operation varied from simple localexcision (n = 4) to total gastrectomy (n = 1). Most commonwas partial gastrectomy, usually antrectomy (n = 12), followedby wedge resection (n = 11). Seven patients had subtotalgastrectomy. Two patients underwent total gastrectomy upongastric recurrence 15 and 30 years after the primary tumor.
PathologySelected pathologic features are shown in Table 1. The
tumor size varied form 1.5 cm to 24 cm (median, 6 cm). In4 cases, the size of the primary tumor was not available, buttwo of these tumors were known to be over 10 cm.
Representative images are shown in Figure 2. Histo-logically, the majority of the tumors (26 of 44, 76%) had purelyor predominantly epithelioid morphology; 6 of these caseshad focal spindle cell areas. The epithelioid tumors varied frommoderately to highly cellular and were most commonly sub-classified as hypercellular (n = 18) based on densely packedcells yet lacking sarcomatous features by low-mitotic rate;4 epithelioid tumors were overtly sarcomatous with high mi-totic activity, 3 sclerosing, and 1 of discohesive subtype. Twelvetumors had purely or predominantly spindle cell pattern, and4 of these cases had focal epithelioid cytology. The spindle celltumors were subtyped as sclerosing (n = 2), palisading-vacuolated(n = 4), hypercellular (n = 3), and sarcomatous (n = 3). Sixtumors contained mixed epithelioid and spindle cell compo-nents and did not fit into subclassification.
The mitotic rate varied from 0/50 to 65/50 HPFs (me-dian 6/50 HPFs). Typical feature in these tumors were muscleinvasion between gastric smooth muscle fibers (34 cases); thisoften created a plexiform growth pattern with alternating areasof tumor and normal smooth muscle. Perinuclear vacuolizationwas also typical, seen in 30 cases. Seven epithelioid tumorshad well or partially developed organoid pattern (Fig. 2A)and 7 spindle cell tumors but none of the epithelioid tumorsshowed nuclear palisading resembling that commonly seen inschwannoma (Fig. 2E).
Coagulative necrosis (2 cases) and mucosal invasion(1 case) were rare findings, but foci of liquefactive necrosisoften seen in adult GISTs were not present. None of the tumorshad calcification. Lymph nodes were negative in all 8 cases inwhich nodes were sampled.
Immunohistochemically, all but one of the 24 casestested for KIT (CD117) were positive (96%) typically showingstrong pan-cytoplasmic staining highlighting the tumoralelements from fibrovascular background (Fig. 2G, H). CD34was present in 21 of 25 cases (84%), typically extensively(Fig. 2I), but smooth muscle actin (Fig. 2J), desmin, and S-100protein in none of the 24 cases tested.
Molecular GeneticsAll 13 tumors analyzed (7 of them 8- to 16-year-old girls)
showed wild-type sequences of KIT exons 9, 11, 13, and17, and wild-type sequences of PDGFRA exons 12 and 18.
Follow-UpThe data are summarized in Table 1. Follow-up infor-
mation was available of 32 patients. A total of 21 patients werealive with no evidence of disease with median follow-up of17 years (range, 741 years). Five patients were alive with livermetastasis with median follow-up time of 14 years (range, 922 years). Six patients died of disease (liver metastases) withmedian survival of 16 years (range, 5.535.5 years).
DISCUSSIONGastric GISTs are rare in children and encompass a
spectrum of clinically benign and malignant tumors. Mostcommonly gastrointestinal cancer in children represents alymphoma. However, two studies3,36 found that 2 of 3 and 2 of8 gastric malignancies, respectively, were sarcomas, probablyrepresenting GISTs in the current classification.
Patients at or under the age 16 represent 1.4% and thoseunder the age of 21 years represent 2.5% of all gastric GISTpatients in our series; it is possible that this number overstatesthe frequency of childhood tumors because of consultationbias; a similar frequency was found in an older AFIP serieson gastric epithelioid GISTs.1 However, two recent series of76 and 108 gastric GISTs did not include any children.50,51 Inthe AFIP series of GISTs of other sites, only 1 of 132 rectaland 1 of 156 duodenal GISTs (,1%) occurred in patients at orunder the age of 21 year indicating that intestinal GISTs aremuch less common than the gastric ones at young age.38,39
Based on our series and previously published cases(summarized and referenced in Table 2), a majority of gastricGISTs below the age of 16 years occurs in girls; in our seriesall but 1 of the patients were female. This suggests a devel-opmentally related sex difference, with the occurrence in malesbeing essentially restricted to postpubertal age. According toour findings, GISTs at young age are not associated with NF1or familial occurrence, neither of which was encountered amongthe 44 patients in this study. Only 1 patient in our series hasevidence of Carney triad, suggesting that this syndrome is notassociated with the majority of GISTs of early onset; amongthe 38 previously published cases, 7 (18%) had Carney triad(Table 2). Nevertheless, there is close demographic similarityin the pediatric gastric GIST patients with or without signs orCarney triad, suggesting that these groups may be related.
Certain clinicopathologic features were associated withchildhood GISTs in this series: epithelioid cytology with highcellularity, and location in the antrum in a majority of cases;of all gastric GISTs only 29% occurred in the antrum.40 Pre-viously reported childhood gastric GISTs also had epithelioidcytology in a majority of cases, and antrum and pylorus werecommon locations (cited in Table 2).
Although GISTs in general are known to have KIT orPDGFRA activating mutations with an overall high frequency,none of the 11 subjects in this study had such mutations. Thisstrongly suggests that the pathogenesis of GIST in young age
1376 q 2005 Lippincott Williams & Wilkins
Miettinen et al Am J Surg Pathol Volume 29, Number 10, October 2005
-
8/12/2019 GIST NIOS
5/9
FIGURE 2. Typical examples of gastricGISTs in children in young adults. A,Epithelioid GIST with an organoidpattern with superficial resemblanceto paraganglioma. B, Hypercellularepithelioid GIST with pseudorosettes.C, Hypercellular epithelioid GIST witha focal trabecular pattern. D, Sarco-matous epithelioid GIST with a signif-icant mitotic activity. E, Spindle cell
GIST of palisading vacuolized subtype.F, Hypercellular spindle cell GIST.G, Strongly KIT-positivegastric GIST. H,Strongly KIT-positive gastric GIST. I,Strongly CD34-positive gastric GIST.J, All tumors were negative for smoothmuscle actin.
q 2005 Lippincott Williams & Wilkins 1377
Am J Surg Pathol Volume 29, Number 10, October 2005 Gastric GISTs in Children
-
8/12/2019 GIST NIOS
6/9
TABLE 2. Summary of 38 Previously Published Cases of Gastric GISTs/GANTs in Children and Young Adults
Case No. Age (yr) Sex Tumor Size (cm) Location Mitoses/HPF
1 3.5 F 3 0/50
2 4 M 5.7 3 4.8 3 4.3 Fundus ,2/HPF
3 7 F 4 3 4 Antrum, posterior wall Easily found
5 9 F Large Distal stomach 5/10
6 10 F 8 3 5 (rec) Posterior wall, LC ND
7 10 F Multiple, ad 2 cm 0/50
8 10 F 8 LC 2/10
9 10 F 5.5 3 3.4 3 1.5 Fundus, posterior
10 10 M 6.5 3 5.5 3 3 Antrum, anterior wall 30/50
11 11 F 8.5 LC 15/10
12 11 F 18.5 3 16 3 11 GC 7/50
13 11 F 11.0 Body and antrum 8/50
14 11.5 F 5.5 3 2.5 25/50
18 11.7 F 4.5 LC
15 11 M 12 3 10 LC
16 11 M 12 3 9 3 6 Near pylorus, GC 1/10
17 12 F 13 3 4.5 LC 5-6/50
19 13 F Large rare
20 13 F 3.8 Antrum, posterior wall 28/10
21 13 F Huge, .15 Antrum, LC ,5/50
22 13 F 8 cm+, multiple nodules Near cardia, antrum 0/50
23 13 M Pylorus
24 14 F 8.0 Body, posterior wall 14/50
25 14 F Large, multinodular 2/50
26 15 F 10 Antrum, LC ,1/50
27 15 F 0.52.7, multiple nodules Pylorus 1/25
28 15 F 16 cm, multiple
29 15 M 9.0 Body and antrum 4/50
30 15 M 32 3 24 3 15 250/50
31 16 F 0.25 multiple nodules Fundus, body, duodenum ,1/20
32 16 F 15 3 8, multiple nodules Midbody to pylorus, LC
33 16 F 5.0 Distal stomach 3/10
34 16 M 8 3 8 3 7 LC 4/50
35 17 F 7 cm (estimated)
36 17 F
37 17 F 1/50
38 19 F Multiple
Case No. Cell Type KIT Comment Follow-Up (yr) Outcome Reference
1 S 1 yr DOD, liver mets 54
2 E + 13
3 E 47
5 E + 0.5 AWD, liver mets* 13
6 E/S 8.5 ANED, rec at 8 yr 13
7 Diagnosed as GANT 1.3 ANED 30
8 Diagnosed as GANT 8.7 ANED 22
9 S 18.0 ANED 36, 5310 E/S + 15
11 Diagnosed as GANT 1.6 ANED 22
12 S + 1.5 ANED 15
13 E 18.0 AWD, liver mets 21
14 E + 12.7 ANED 10
18 S/E 4.3 ANED, with treated liver mets 20
1378 q 2005 Lippincott Williams & Wilkins
Miettinen et al Am J Surg Pathol Volume 29, Number 10, October 2005
-
8/12/2019 GIST NIOS
7/9
groups may differ from that in adults. Previously another sub-group of GISTs, those occurring in neurofibromatosis 1 pa-tients, has been reported to be negative for KIT and PDFGRAmutations.23 Recently, one gastric GIST in an adult with Carneytriad12 and another, pediatric one without it33 were also foundnegative for KIT and PDGFRA mutations. If the KIT/PDGFRAmutation negativity applies to Carney triad-associated GISTsin general, pediatric gastric GISTs with or without Carney triadmay have a similar pathogenesis, possibly involving alterna-tive mode of KIT activation than the type of mutationstypically seen in GISTs. More studies are needed to under-stand the pathogenesis of pediatric gastric GISTs.
The occurrence of GISTs at young age raises thequestion whether this could be linked with familial disease.However, none of our patients, including 19 patients who wereinterviewed, had evidence of GISTs in other family members.Also, there are many differences between pediatric and reported
familial GISTs. The latter manifest in adult age (age range in23 patients with reported details, 1871 years; median, 45 years),and are always associated with constitutional KIT or PDGFRAmutation.2,5,9,18,19,32,35,41,45 In two studies, occurrence in chil-dren of the affected families was specifically excluded, in 1 caseby CT scan.2,32 No KIT or PDGFRA mutations were detectedin pediatric GISTs, indicating a different pathogenesis.
Prognostically, gastric GISTs in children are heteroge-neous. A majority of these tumors are clinically indolent withan excellent long-term prognosis, based on our cases with variablylong follow-up and previously published cases with mostlylimited follow-up (Table 2). Treatable recurrences are not un-common and may reflect initial insufficient excision or multi-focal disease escaping surgical detection at the outset.
In our series 11 of 32 patients with follow-up developedliver metastases, and 6 patients died during the follow-up. Mostof the patients who developed metastases were in unfavorable
TABLE 2. (continued) Summary of 38 Previously Published Cases of Gastric GISTs/GANTs in Children and Young Adults
Case No. Cell Type KIT Comment Follow-Up (yr) Outcome Reference
15 S 0.5 DOD, abdominal and liver mets
36, 53
16 S 2.0 ANED 34
17 E + AWD, liver mets 33
19 7.0 AWD, peritoneal implantsat 5 yr
54
20 Diagnosed as GANT 0.7 ANED 22
21 E 1.0 ANED 42
22 1.2 AWD, liver mets 54
23 S/E + Monozygotic twin had retroperitoneal paraganglioma
AWD, liver mets 4
24 E 6.0 AWD, liver mets 26
25 54
26 E Also pulmonary chondroma 27.0 ANED, abdominal rec/mets at 9, 16, 20, 25 yr
44
27 S 0.8 AWD, liver mets 25
28 E Also mediastinalparaganglioma
1.5 ANED 14
29 5.0 ANED 26
30 S + 1.3 ANED* 10
31 E Also mediastinalparaganglioma
2.5 ANED 43
32 E/S Also pulmonary chondromaand mediastinal
paraganglioma
9 ANED 11
33 Diagnosed as GANT 9.0 ANED, recurrence, with LNinvolvement at 3 and 5 yr
22
34 S Features of GANT, Alsoretroperitoneal
paraganglioma
0.7 ANED 49, 52
35 + Survivor of a neuroblastomaat the age of 5 mo
1.1 ANED 21
36 E Also retroperitonealparaganglioma
6
37 E 4838 Also 3 para-aortic
paragangliomas6
LC, lesser curvature; GC, greater curvature; mets, metastases; rec, recurrence; ANED, alive with no evidence of disease; AWD, alive with disease; DOD, dead of disease.
*Patient has received imatinib mesylate for treatment. In some cases, age has been rounded to the closest year.
q 2005 Lippincott Williams & Wilkins 1379
Am J Surg Pathol Volume 29, Number 10, October 2005 Gastric GISTs in Children
-
8/12/2019 GIST NIOS
8/9
categories with high mitotic rate, large tumor size, or both.However, 3 of 13 patients with gastric GISTs with favorableparameters associated with only 2% to 3% mortality in gastricGIST patients in general40 developed metastasis (Table 3).
This may suggest that GISTs in young age are somewhat un-predictable and may behave more aggressively than those inadults, as the comparison with our collective data on gastricGISTs shows.
REFERENCES1. Appelman HD, Helwig EB. Gastric epithelioid leiomyoma and leiomyo-
sarcoma (leiomyoblastoma). Cancer. 1976;38:708728.2. Beghini A, Tibiletti M, Roversi G, et al. Germline mutation in the
juxtamembrane domain of the Kit gene in a family with gastrointestinalstromal tumors and urticaria pigmentosa. Cancer. 2001;92:657662.
3. Bethel CAI, Bhattacharyya, Hutchinson C, et al. Alimentary tract malig-nancies in children. J Pediatr Surg. 1997;32:10041009.
4. Boccon-Gibod L, Boman F, Boudjemaa S, et al. Separate occurrence ofextra-adrenal paraganglioma and gastrointestinal stromal tumor in mono-
zygotic twins: probable familial Carney syndrome. Pediatr Dev Pathol.2004;7:380384.5. Carballo M, Roig I, Aguilar F, et al. Novel c-KIT germline mutation in
a family with gastrointestinal stromal tumors and cutaneous hyperpig-mentation.Am J Med Genet. 2005;132:361364.
6. Carney JA, Sheps SG, Go VL, et al. The triad of gastric leiomyosarcoma,functioning extra-adrenal paraganglioma and pulmonary chondroma.
N Engl J Med. 1977;296:517518.7. Carney JA. Gastric stromal sarcoma, pulmonary chondroma, and extra-
adrenal paraganglioma (Carney triad): natural history, adrenocorticalcomponent, and possible familial occurrence. Mayo Clin Proc. 1999;74:543552.
8. Carney JA, Stratakis CA. Familial paraganglioma and gastric stromal sar-coma: a new syndrome distinct from the Carney triad. Am J Med Genet.2002;108:132139.
9. Chompret A, Kannengiesser C, Barrois M, et al. PDGFRA germlinemutation in a family with multiple cases of gastrointestinal stromal tumor.
Gastroenterology. 2004;126:318321.10. Cypriano MS, Jenkins JJ, Pappo AS, et al. Pediatric gastrointestinalstromal tumors and leiomyosarcoma. Cancer. 2004;101:3950.
11. de Castro FJ, Olsen WR,Littler ER. Gastricleiomyoblastoma in an adolescent.Am J Surg. 1972;123:614616.
12. Diment J, Tamborini E, Casali P, et al. Carney triad: case report andmolecular analysis of gastric tumor. Hum Pathol. 2005;36:112116.
13. Durham MM, Gow KW, Shehata BM, et al. Gastrointestinal stromaltumors arising from the stomach: a report of three children.J Pediatr Surg.2004;39:14951499.
14. Grace MP, Batist G, Grace WR, et al. Aorticopulmonary parangangliomaand gastric leiomyoblastoma in a young woman. Am J Med. 1981;70:12881292.
15. Haider N, Kader M, McDermott M, et al. Gastric stromal tumors inchildren.Pediatr Blood Cancer. 2004;42:186189.
16. Heinrich MC, Corless CL, Duensing A, et al. PDGFRA activatingmutations in gastrointestinal stromal tumors.Science. 2003;299:708710.
17. Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kitin human gastrointestinal stromal tumors.Science. 1998;279:577580.
18. Hirota S, Nishida T, Isozaki K, et al. Familial gastrointestinal stromaltumors associated with dysphagia and novel type germline mutation of
KIT gene. Gastroenterology. 2002;122:14931499.19. Isozaki K, Terris B, Belghiti J, et al. Germline-activating mutation in thekinase domain of KIT gene in familial gastrointestinal stromal tumors.Am
J Pathol. 2000;157:15811585.20. Johnson H, Hutter JJ Jr, Paplanus SH. Leiomyosarcoma of the stomach:
results of surgery and chemotherapy in an eleven-year-old girl with livermetastases.Med Pediatr Oncol. 1980;8:137142.
21. Johnston DL, Olson JM, Benjamin DR. Gastrointestinal stromal tumor ina patient with previous neuroblastoma. J Pediatr Hematol Oncol. 2001;23:255256.
22. Kerr JZ, Hicks MJ, Nuchtern JG, et al. Gastrointestinal autonomic nervetumors in the pediatric population: a report of four cases and reviewof theliterature. Cancer. 1999;85:220230.
23. Kinoshita K, Hirota S, Isozaki K, et al. Absence of c-kit gene mutations ingastrointestinal stromal tumours from neurofibromatosis type 1 patients.
J Pathol. 2004;202:8085.24. Kitamura Y, Hirota S, Nishida T. Molecular pathology of c-kit proto-
oncogene and development of gastrointestinal stromal tumors. Ann ChirGynaecol. 1998;87:282286.25. Kodet R, Snajdauf J, Smelhaus V. Gastrointestinal autonomic nerve
tumor: a case report with electron microscopic and immunohistochemicalanalysis and review of the literature.Pediatr Pathol. 1994;14:10051016.
26. Lack EE. Leiomyosarcomas in childhood: a clinical and pathologic studyof 10 cases. Pediatr Pathol. 1986;6:181197.
27. Lasota J, Jasinski M, Sarlomo-Rikala M, et al. C-kit mutations occurpreferentially in malignant vs. benign gastrointestinal stromal tumors anddo not occur in leiomyomas and leiomyosarcomas. Am J Pathol. 1999;154:5360.
28. Lasota J, Wozniak A, Sarlomo-Rikala M, et al. Mutations in exons 9 and13 of KIT gene are rare events in gastrointestinal stromal tumors: a studyof two hundred cases. Am J Pathol. 2000;157:10911095.
29. Lasota J, Dansonka-Mieszkowska A, Sobin LH, et al. A great majority ofGISTs with PDGFRA mutations represents gastric tumors of no or lowmalignant potential. Lab Invest. 2004;84:874883.
30. Lauwers GY, Erlandson RA, Casper ES, et al. Gastrointestinal autonomicnerve tumors: a clinicopathological, immunohistochemical, and ultra-structural study of 12 cases. Am J Surg Pathol. 1993;17:887897.
31. Lee JR, Joshi V, Griffin JW Jr, et al. Gastrointestinal autonomic nervetumor: immunohistochemical and molecular identity with gastrointestinalstromal tumor. Am J Surg Pathol. 2001;25:979987.
32. Li FP, Fletcher JA, Heinrich MC, et al. Familial gastrointestinal stromaltumor syndrome: phenotypic and molecular features in a kindred.J ClinOncol. 2005;23:27352743.
33. Li P, Wei J, West AB, et al. Epithelioid gastrointestinal stromal tumor ofstomach with liver metastases in a 12-year old girl: aspiration cytologyand molecular study. Pediatr Dev Pathol. 2002;5:386394.
34. Luzzatto C, Calligioni A, Candiani F, et al. Gastric leiomyoblastoma inchildhood: a case report and review of the literature. Z Kinderchir. 1989;44:373376.
35. Maeyama H, Hidaka E, Ota H, et al. Familial gastrointestinal stromaltumor with hyperpigmentation associated with a germline mutation of the
c-kit gene. Gastroenterology. 2001;120:210215.36. Mahour GH, Isaacs H Jr, Chang L. Primary malignant tumors of thestomach in children. Pediatr Surg. 1980;15:603608.
37. Miettinen M, Lasota J. Gastrointestinal stromal tumors: definition, clin-ical, histological, immunohistochemical, and molecular genetic featuresand differential diagnosis. Virchows Arch. 2001;438:112.
38. Miettinen M, Sarlomo-Rikala M, Sobin LH, et al. Gastrointestinal stromaltumors of the rectum: a clinicopathologic, immunohistochemical and mo-lecular genetic study of 144 cases.Am J Surg Pathol. 2001;25:11211133.
39. Miettinen M, Kopczynski J, Maklouf HR, et al. Gastrointestinal stromaltumors, intramural leiomyomas and leiomyosarcomas in the duodenum:a clinicopathologic, immunohistochemical and molecular genetic study of167 cases. Am J Surg Pathol. 2003;27:625641.
TABLE 3. Prognosis of 30 GISTs in Children and YoungAdults by Prognostic Groups in Comparison With 1055Gastric GIST Patients
Patients WithMetastases of All in the Group (%)
Prognostic Group
and Definition
Children and
Young Adults
All Gastric
GIST Patients2 (#5 cm, #5/50 HPF) 1/6 (17%) 6/320 (2%)
3A (5 # 10 cm, #5/50 HPF) 2/7 (28%) 8/229 (3%)
3B (.10 cm, #5/50 HPF) 1/2 (50%) 17/140 (12%)
5 (.2 # 5 cm, .5/50 HPF) 1/7 (14%) 16/99 (16%)
6A (.5 # 10 cm, .5/50 HPF) 3/5 (60%) 52/96 (54%)
6B (.10 cm, .5/50 HPF) 2/3 (67%) 89/108 (82%)
Note: Only cases with follow-up and defined tumor size are included.
1380 q 2005 Lippincott Williams & Wilkins
Miettinen et al Am J Surg Pathol Volume 29, Number 10, October 2005
-
8/12/2019 GIST NIOS
9/9
40. Miettinen M, Sobin LH, Lasota J. Gastrointestinal stromal tumors ofthe stomach: a clinicopathologic, immunohistochemical, and moleculargenetic studies of 1765 cases with long-term follow-up.Am J Surg Pathol.2005;29:5268.
41. Nishida T, Hirota S, Taniguchi M, et al. Familial gastrointestinal stromaltumours with germline mutation of the KIT gene. Nat Genet. 1998;19:323324.
42. Oguzkurt P, Akcoren Z, Sonocak ME, et al. A huge gastric stromal tumor
in a 13-year-old girl. Turk J Pediatr. 2002;44:6568.43. Perez-Atayde AR, Shamberger RC, Kozakewich HW. Neuroectodermaldifferentiation of the gastrointestinal tumors in the Carney triad: anultrastructural and immunohistochemical study.Am J Surg Pathol. 1993;17:706714.
44. Persson S, Kindblom LG, Angervall L, et al. Metastasizing gastricepithelioid leiomyosarcomas (leiomyoblaastomas) in young individualswith long-term survival. Cancer. 1992;70:721732.
45. Robson ME, Glogowski E, Sommer G, et al. Pleomorphic characteristicsof a germ-line KIT mutation in a large kindred with gastrointestinal stromaltumors, hyperpigmentation, and dysphagia. Clin Cancer Res. 2004;10:12501254.
46. Rubin BP, Singer S, Tsao C, et al. KIT activation is ubiquitous feature ofgastrointestinal stromal tumors. Cancer Res. 2001;61:81188121.
47. Schmitt EL, Heidelberger KP. Gastric leiomyoblastoma in a child. J CanAssoc Radiol. 1976;27:115117.
48. Stout AP. Bizarre smooth muscle tumors of the stomach.Cancer. 1962;15:400409.
49. Tortella BJ, Matthews JB, Antonioli DA, et al. Gastric autonomic nerve(GAN) tumor and extra-adrenal paraganglioma in Carneys triad:a common origin. Ann Surg. 1987;205:221225.
50. Trupiano JK, Stewart RE, Misick C, et al. Gastric stromal tumors: a
clinicopathologic study of 77 cases with correlation of features with non-aggressive and aggressive behaviors. Am J Surg Pathol. 2002;26:705714.
51. Wong NACS, Young R, Malcolmson RDG, et al. Prognostic indicators forgastrointestinal stromal tumours: a clinicopathological and immunohis-tochemical study of 108 resected cases of the stomach. Histopathology.2003;43:118126.
52. Walker P, Dvorak AM. Gastrointestinal autonomic nerve tumor: ultra-structural evidence for a newly recognized entity. Arch Pathol Lab Med.1986;110:309316.
53. Wurlitzer FP, Mares AJ, Isaacs H Jr, et al. Smooth muscle tumors of thestomach in childhood and adolescence.J Pediatr Surg. 1973;8:421427.
54. Yannopoulos K, Stout AP. Smooth muscle tumors in children. Cancer.1962;15:958971.
q 2005 Lippincott Williams & Wilkins 1381
Am J Surg Pathol Volume 29, Number 10, October 2005 Gastric GISTs in Children